Warfarin and Antibiotics: How Broad-Spectrum Antibiotics Raise INR and Increase Bleeding Risk

Warfarin Antibiotic Safety Checker
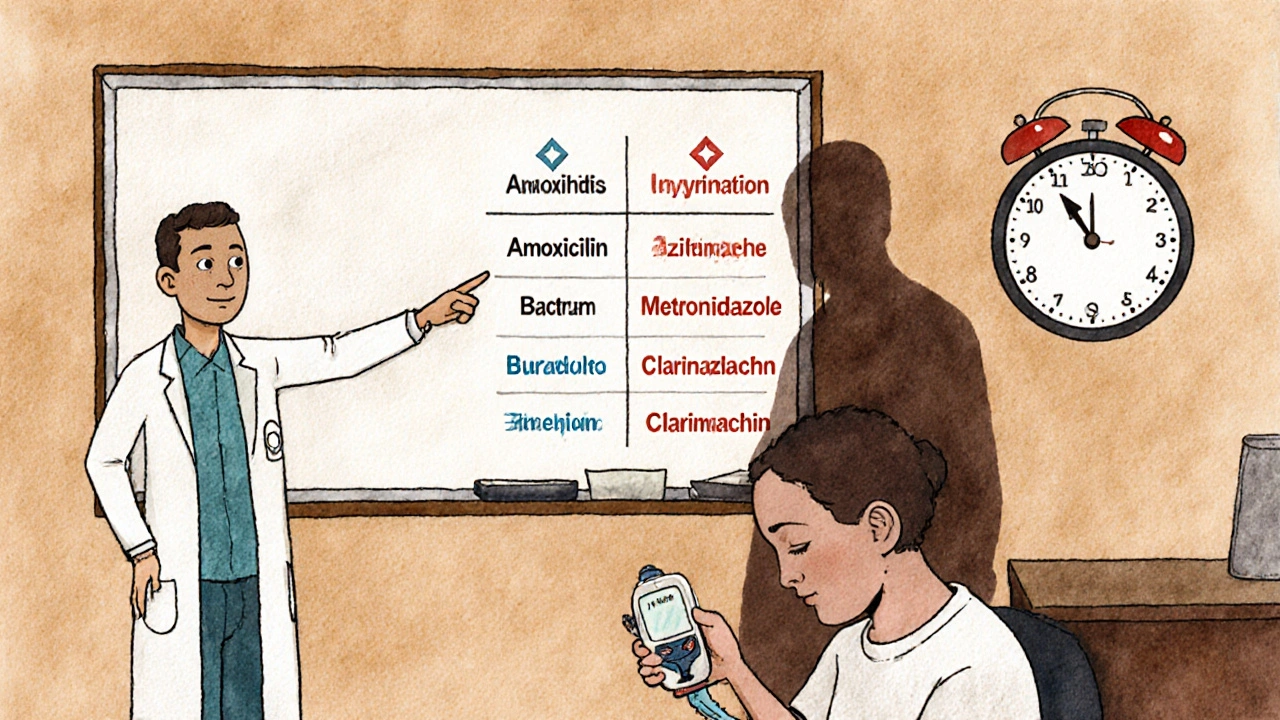
Check Antibiotic Safety for Warfarin Users
Select your antibiotic to determine risk level and recommended INR monitoring schedule.
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance - sometimes dangerously so. You might think a quick course of amoxicillin for a sinus infection is harmless, but for millions of people taking warfarin, that’s not the case. The interaction between warfarin and certain antibiotics can cause your INR to spike overnight, turning a routine prescription into a medical emergency. This isn’t theoretical. It’s happening in clinics, ERs, and homes across the country - and most people don’t see it coming.
Why Warfarin Is So Sensitive
Warfarin doesn’t just thin your blood. It works by blocking vitamin K, which your body needs to make clotting factors. Too little, and you bleed. Too much, and clots form. The sweet spot? An INR between 2.0 and 3.0. Go above 5.0, and your risk of serious bleeding - brain hemorrhage, internal bleeding, GI bleeds - jumps dramatically. That’s why warfarin has a narrow therapeutic index. A tiny change in dose or metabolism can push you out of safety.
Here’s the catch: warfarin is broken down by liver enzymes - mainly CYP2C9, CYP3A4, and CYP1A2. Many antibiotics interfere with these enzymes. Some block them. Others speed them up. And then there’s the gut.
Your intestines host bacteria that make about 10-15% of your daily vitamin K. When antibiotics wipe out those bugs, vitamin K drops. That means warfarin works harder. No extra dose needed. Just a few days of antibiotics, and your INR climbs.
Not All Antibiotics Are Created Equal
Some antibiotics barely touch your INR. Others? They’re landmines.
- High-risk: Fluoroquinolones like levofloxacin and ciprofloxacin, macrolides like clarithromycin, sulfonamides like trimethoprim-sulfamethoxazole (Bactrim), and metronidazole. These can push INR up by 1.5 to 4 points in under a week. In one study, 31% of patients on metronidazole saw INR spikes above 5.0.
- Moderate-risk: Some cephalosporins and high-dose IV penicillins. Rare, but possible. Case reports exist.
- Low-risk: Amoxicillin, ampicillin, azithromycin. These rarely affect INR. Azithromycin, in particular, shows no significant interaction in over 98% of cases.
Here’s the problem: doctors often don’t know the difference. A 2020 study found only 48% of primary care providers could correctly identify which antibiotics were dangerous with warfarin. Many assume all antibiotics are safe - until a patient shows up in the ER with a bleeding ulcer and an INR of 8.2.
The Delayed Effect You Can’t Ignore
Unlike most drug interactions that happen right away, warfarin-antibiotic effects creep in. You start amoxicillin on Monday. Nothing changes. Wednesday? Still fine. By Friday? INR jumps from 2.4 to 5.1. You’re confused. You didn’t change your warfarin dose. Why now?
The delay comes from two sources:
- Gut flora disruption: Killing vitamin K-producing bacteria takes 3-7 days to fully impact your levels.
- Enzyme inhibition: CYP2C9 blockers like clarithromycin slow warfarin clearance. Warfarin’s half-life stretches from 36 hours to over 60. It builds up slowly.
That’s why checking INR the day after starting an antibiotic is useless. You need to wait. Most guidelines say: check at day 3-5. But for high-risk antibiotics like levofloxacin or Bactrim, wait until day 7. That’s when the full effect hits.
What Happens When You Stop the Antibiotic?
It’s not just about starting antibiotics. Stopping them can be just as dangerous.
Once you stop a CYP inhibitor like clarithromycin, your liver enzymes spring back to life. Warfarin gets cleared faster. Your INR plummets. Within 3-5 days, it can drop from 2.8 to 1.2. That’s no longer therapeutic. That’s a stroke risk.
One Reddit thread from r/Anticoagulation described two patients who had strokes after stopping ciprofloxacin. Their INR had crashed. They thought they were fine - no bleeding, no symptoms. But clots were forming silently.
That’s why guidelines say: check INR again 7-10 days after finishing the antibiotic. You might need to increase your warfarin dose back up. Not decrease. The body rebounds.
Who’s Most at Risk?
Not everyone on warfarin reacts the same way. Some people are walking time bombs.
- Age 75+: Liver function declines. Metabolism slows. Warfarin lingers longer.
- Cancer patients: Cancer itself alters drug metabolism. One study showed cancer patients were nearly twice as likely to have dangerous INR spikes.
- Women: Hormonal differences affect enzyme activity. Women have a 42% higher risk of INR >5.0 after antibiotic use.
- Baseline INR >2.5: If you’re already near the top of your therapeutic range, even a small bump can push you over the edge.
These aren’t rare cases. In the 2014 JAMA study of over 13,000 patients, nearly 1 in 3 who had an INR above 5.0 had all three risk factors: older, female, with cancer.
What You Should Do - Step by Step
If you’re on warfarin and your doctor prescribes an antibiotic, here’s what you need to do:
- Ask: “Is this antibiotic safe with warfarin?” Don’t assume. Bring up the list: fluoroquinolones, Bactrim, metronidazole, clarithromycin. If they say “probably fine,” push back.
- Get an INR check 3-5 days after starting the antibiotic. If it’s high-risk, wait until day 7.
- Don’t wait for symptoms. Bleeding starts quietly - bruising, nosebleeds, dark stools, headaches. By the time you feel it, it’s too late.
- Check INR again 7-10 days after stopping the antibiotic. Your dose might need to go back up.
- Consider switching antibiotics. If you need an antibiotic, ask if azithromycin or amoxicillin is an option. They’re safer.
Some patients now use home INR monitors - devices like the Roche CoaguChek INRange - that connect to smartphones. These let you test daily during antibiotic therapy. If you’re high-risk, ask your doctor about getting one.

The Bigger Picture
Warfarin is still used by over 3 million Americans. Why? It’s cheap. $4.27 a month. Versus $527 for apixaban. For Medicare patients, that’s the difference between staying on warfarin or going without anticoagulation.
But cost comes with risk. Every year, warfarin-antibiotic interactions cause over 1,200 deaths and $1.2 billion in preventable healthcare costs in the U.S. The FDA now requires all antibiotic labels to warn about warfarin interactions. But warnings don’t change behavior.
Doctors still prescribe Bactrim for UTIs in elderly patients on warfarin. Pharmacists still dispense it without flagging it. Patients still take it without knowing the danger.
The real solution? Better education. Better communication. And never assuming an antibiotic is “safe.”
When to Call Your Doctor Immediately
Even if you’re following all the rules, something can go wrong. Call your anticoagulation clinic or go to the ER if you notice:
- Bleeding that won’t stop (nose, gums, cuts)
- Unexplained bruising or purple spots on skin
- Dark, tarry stools or blood in urine
- Sudden severe headache, dizziness, confusion
- Unusual swelling or pain in limbs
These aren’t side effects. They’re warning signs of internal bleeding. INR could be above 8.0. You might need vitamin K or a plasma transfusion. Don’t wait.
Can I take amoxicillin while on warfarin?
Yes, amoxicillin is generally safe with warfarin. It doesn’t significantly affect liver enzymes or gut bacteria that produce vitamin K. Most patients see no change in INR. Still, it’s smart to check your INR 5 days after starting any new medication - just to be sure.
Does azithromycin affect INR?
No, azithromycin does not meaningfully affect INR. Unlike other macrolides like clarithromycin, it doesn’t inhibit CYP enzymes. Multiple studies show no significant change in INR in over 98% of patients taking azithromycin with warfarin. It’s often the preferred antibiotic choice for people on anticoagulants.
How long after stopping an antibiotic should I check my INR?
Check your INR 7-10 days after stopping an antibiotic that interacts with warfarin. When you stop the drug, your liver enzymes rebound, and warfarin clears faster. This can cause your INR to drop below the therapeutic range, increasing stroke risk. Waiting until day 7-10 gives your body time to reset.
Can I take over-the-counter antibiotics with warfarin?
There are no true over-the-counter antibiotics in the U.S. All antibiotics require a prescription. But if you’re using herbal supplements or foreign medications labeled as “antibiotics,” they can still interact. Avoid any unregulated products. Stick to what your doctor prescribes.
Why do some people have big INR spikes while others don’t?
Genetics play a big role. People with certain CYP2C9 gene variants (like CYP2C9*2 or *3) break down warfarin much slower. If they take a CYP inhibitor like metronidazole, warfarin builds up fast. Age, liver health, diet (especially vitamin K intake), and other medications also matter. One person might take Bactrim with no change, while another’s INR jumps from 2.6 to 7.8.
Are there alternatives to warfarin that don’t interact with antibiotics?
Yes - direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran have far fewer drug interactions. They don’t rely on vitamin K or CYP enzymes the same way warfarin does. Most antibiotics don’t affect them. But DOACs are expensive and not always covered by insurance. For many Medicare patients, warfarin remains the only affordable option - which makes understanding interactions even more critical.
Final Thought: Don’t Guess. Test.
Warfarin isn’t going away. It’s too cheap, too effective for certain conditions, and too deeply embedded in the healthcare system. But its dangers are real - and preventable. The difference between safety and disaster often comes down to one thing: checking your INR at the right time.
If you’re on warfarin, treat every antibiotic like a potential trigger. Ask questions. Get tested. Don’t wait for bleeding to happen. Your life might depend on it.
Been on warfarin for 8 years now, and this post hit home. My doc once prescribed Bactrim for a UTI and I didn’t know better - ended up in the ER with an INR of 7.9. No bleeding, just pure luck. Now I always ask about antibiotics like they’re dynamite. Azithromycin is my go-to now. Worth the extra cost if it keeps me alive.
This is one of the most important posts I've read this year. I work in a clinic and see this exact scenario play out every month. Patients think, 'It's just an antibiotic,' and doctors assume it's safe unless it's flagged. The fact that 48% of PCPs can't identify high-risk antibiotics is terrifying. We need mandatory CDS alerts in EHRs - not just warnings on the label. Lives are being lost because of system failures, not ignorance.
Why are we still using warfarin in 2025? It's like driving a 1987 Corolla with no airbags. DOACs exist. They're safer. Cheaper if you're not on Medicare. Stop pretending warfarin is 'necessary' - it's just lazy.
Everyone's acting like this is some groundbreaking revelation but it's been in the literature since the 90s. You're telling me a 75 year old woman on warfarin takes Bactrim and no one thought to check her INR? The real tragedy isn't the interaction - it's the fact that this keeps happening because medicine is still run by people who think 'common sense' is a clinical guideline. Also amoxicillin is fine but if you're on warfarin and you're getting sinus infections every other month maybe stop ignoring your immune system and get a real workup
My grandma took metronidazole for a dental infection and her INR went from 2.1 to 6.8 in 4 days. No symptoms until she woke up with a massive bruise on her thigh. We didn't know until the ER. After that, we got her a CoaguChek. She tests every other day when she's on antibiotics now. It's not expensive - $120 for the device, $0.50 per strip. Way cheaper than a hospital stay. If you're high-risk, get one. Seriously.
From a clinical pharmacology standpoint, the CYP2C9 polymorphism angle is critical. Patients with *2 or *3 alleles have reduced enzymatic activity - their clearance half-life extends from 36 to 80+ hours. When combined with CYP inhibition from fluoroquinolones or metronidazole, the pharmacokinetic synergy is non-linear. The delayed INR peak at day 5-7 correlates with gut flora depletion kinetics, which is why early testing is misleading. Also, vitamin K dietary intake variability (leafy greens, natto) further modulates this interaction - a confounder often overlooked in primary care.
As someone who's spent 20 years working in NHS anticoagulation clinics, I can tell you this isn't just an American problem. We had a cluster of GI bleeds in Brighton last winter - all elderly patients on warfarin, all prescribed ciprofloxacin for 'possible UTI'. One died. We now have a mandatory alert in our prescribing system that forces a double-check if warfarin is active. It's not perfect, but it cut our adverse events by 62%. The key? Don't trust the algorithm. Trust the patient. And always, always check INR at day 7.
Stop being passive. If your doctor prescribes an antibiotic, ask them to write down the INR check dates on your calendar. If they don't, get a new doctor. This isn't complicated. It's not magic. It's basic safety. And if you're on warfarin and you're not using a home monitor, you're gambling with your life. I've seen too many people ignore this until it's too late. Do the work. Test. Track. Survive.