The Science Behind Halobetasol: How This Powerful Steroid Works on Skin
Halobetasol doesn’t just calm red, itchy skin-it shuts down the body’s inflammatory response at the molecular level. If you’ve been prescribed this medication for psoriasis, eczema, or another stubborn skin condition, you might wonder: how does something so strong actually work? The answer isn’t just "it reduces swelling." It’s a precise, powerful biological takeover that stops your immune system from attacking your own skin.
What Halobetasol Actually Is
Halobetasol propionate is a synthetic corticosteroid, part of the glucocorticoid family. It’s classified as a Class I steroid-the strongest available for topical use. That means it’s not something you use lightly. Unlike over-the-counter hydrocortisone, halobetasol was designed for severe, resistant skin conditions. It’s not an antibiotic. It doesn’t kill bacteria. It doesn’t moisturize. It reprograms your skin’s immune signals.
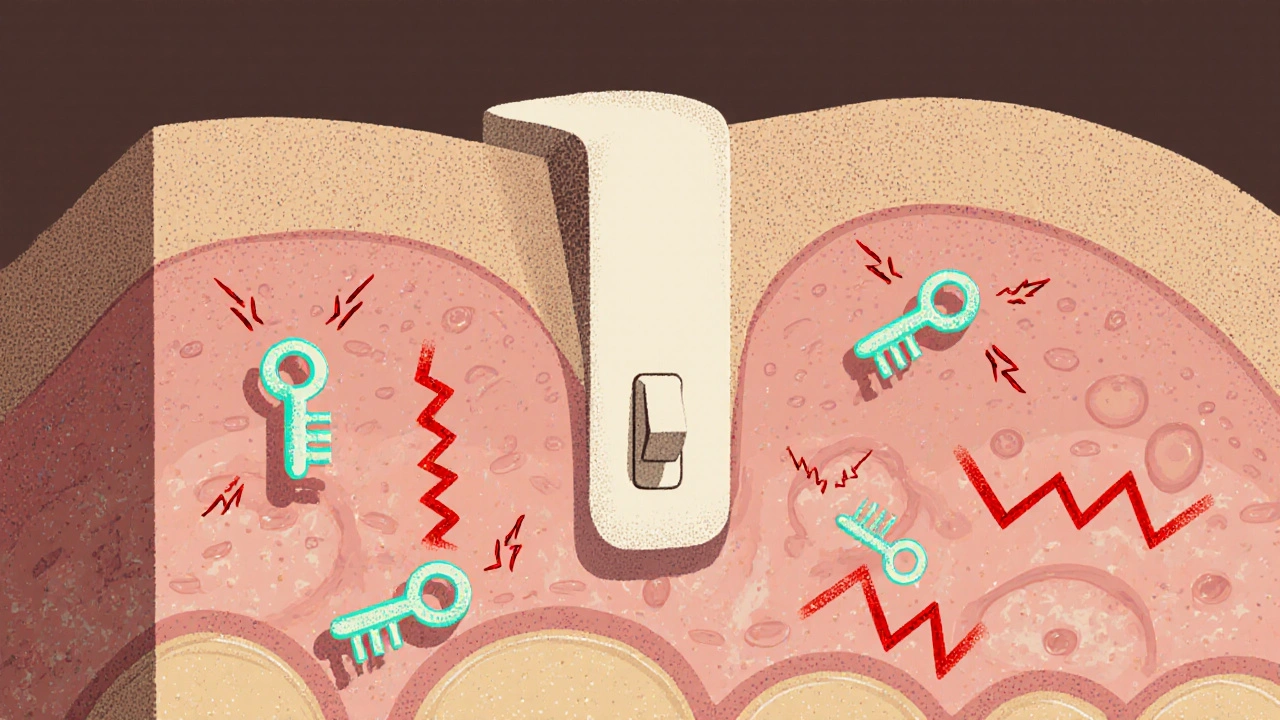
Its chemical structure lets it slip easily through the outer layers of skin and bind tightly to glucocorticoid receptors inside skin cells. Once inside, it acts like a master switch. This switch controls hundreds of genes involved in inflammation, cell growth, and immune activity. When activated, it turns off the genes that make your skin red, swollen, and itchy.
How It Stops Inflammation
When your skin gets irritated-whether from eczema, psoriasis, or an allergic reaction-your body releases inflammatory chemicals like cytokines, prostaglandins, and histamine. These molecules attract immune cells to the area, causing swelling, heat, and pain. In chronic conditions, this process never turns off.
Halobetasol steps in and blocks this chain at multiple points. First, it suppresses the production of those inflammatory chemicals. It does this by binding to glucocorticoid receptors in the nucleus of skin cells. This binding changes how DNA is read, preventing the instructions for making those chemicals from being copied.
Second, it reduces the number of immune cells that show up. T-cells, mast cells, and neutrophils-all key players in skin inflammation-are kept from migrating into the affected area. Without them, the cycle of irritation breaks.
Third, it tightens blood vessels. That’s why your skin looks less red after a few days of use. The narrowed capillaries mean less blood flow to the inflamed zone, which reduces both swelling and the delivery of more immune cells.
Why It Works So Fast-And Why That’s a Double-Edged Sword
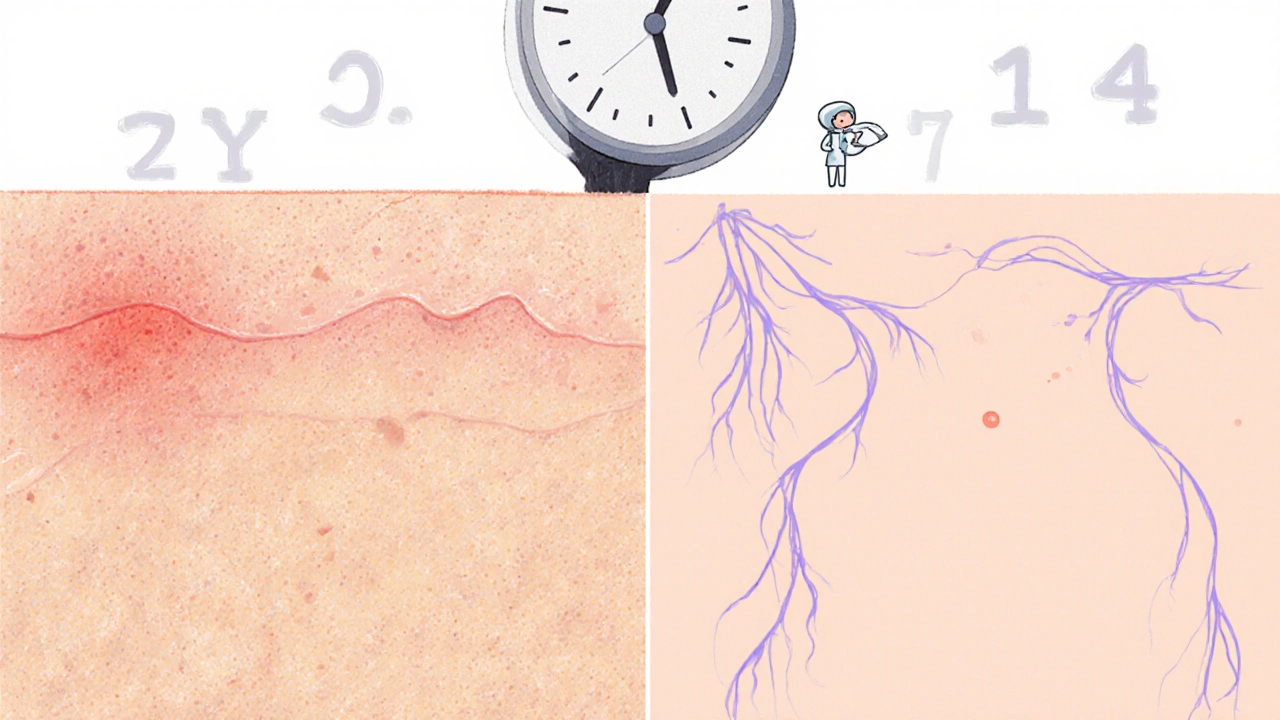
Many people notice improvement in just 24 to 48 hours. That speed is why doctors reach for halobetasol when other treatments fail. But that same speed is why misuse is dangerous.
Unlike weaker steroids that take days to build up effects, halobetasol binds so tightly to receptors that it starts working almost immediately. This makes it effective-but also more likely to cause side effects if used too long or on sensitive areas.
Long-term use can thin the skin. You might notice stretch marks, easy bruising, or visible blood vessels. In rare cases, it can suppress the adrenal glands, which normally produce your body’s natural steroids. That’s why it’s never meant for daily, indefinite use. Most dermatologists prescribe it for no more than two weeks at a time, then switch to a gentler option.

Where It Works Best-and Where It Doesn’t
Halobetasol is most effective on thick, tough skin areas: elbows, knees, scalp, palms, and soles of the feet. These areas absorb the medication well and are often where psoriasis plaques or severe eczema build up.
But it’s a bad fit for thin skin. That includes the face, armpits, groin, and eyelids. Using it there increases the risk of skin atrophy-where the skin becomes paper-thin and fragile. It can also cause acne-like breakouts or perioral dermatitis, especially around the mouth.
Children under 12 shouldn’t use halobetasol unless under strict supervision. Their skin is more permeable, and their bodies are more sensitive to steroid effects. Even in adults, applying it under occlusive dressings (like plastic wrap) can lead to dangerous systemic absorption.
What Happens When You Stop Using It?
Some patients report rebound flares after stopping halobetasol. The skin, having been suppressed, reacts with even more redness and itching than before. This isn’t addiction-it’s a rebound effect. The immune system, suddenly without the steroid’s control, overcompensates.
To avoid this, doctors often recommend tapering. Instead of stopping cold, you might switch to a weaker steroid for a week or use a non-steroidal alternative like pimecrolimus or tacrolimus. Moisturizing daily with ceramide-rich creams also helps rebuild the skin barrier after steroid withdrawal.
How It Compares to Other Steroids
Here’s how halobetasol stacks up against other common topical steroids:
| Steroid | Class | Typical Use | Max Duration | Risk of Skin Thinning |
|---|---|---|---|---|
| Hydrocortisone 1% | Class VII | Mild eczema, diaper rash | Up to 4 weeks | Low |
| Triamcinolone 0.1% | Class IV | Moderate psoriasis, eczema | 2-4 weeks | Moderate |
| Fluocinonide 0.05% | Class II | Severe plaque psoriasis | 2 weeks | High |
| Halobetasol 0.05% | Class I | Resistant psoriasis, chronic eczema | 1-2 weeks | Very High |
Halobetasol is the strongest in this group. It’s not a first-line treatment. It’s reserved for cases where other options have failed. That’s why you won’t find it on drugstore shelves-it requires a prescription.
Real-World Use: What Patients Actually Experience
One 2023 study tracking 1,200 patients with moderate-to-severe plaque psoriasis found that 83% saw significant improvement in scaling and redness after 14 days of daily halobetasol use. But 17% developed mild skin thinning, and 8% reported rebound flare-ups after stopping.
Patients who combined halobetasol with daily emollients reported fewer side effects and longer remission periods. The key wasn’t just the steroid-it was what they did after.
Another common scenario: a patient uses halobetasol on their scalp for psoriasis. After two weeks, the plaques vanish. But if they stop using moisturizer and start using harsh shampoos, the condition returns within weeks. The steroid cleared the inflammation, but didn’t fix the underlying barrier dysfunction.
When to Talk to Your Doctor
You should call your doctor if:
- Your skin becomes shiny, stretched, or transparent
- You develop purple or red streaks (striae)
- Your acne worsens or you get small bumps around your mouth
- You feel unusually tired, dizzy, or nauseated (possible adrenal suppression)
- The condition returns worse than before after stopping
These aren’t rare. They’re predictable outcomes of improper use. Halobetasol is powerful-but it’s not magic. It works best when used like a scalpel: precisely, briefly, and with a plan for what comes next.
What Comes After Halobetasol?
After a short course, the goal isn’t to keep using it-it’s to maintain results without it. Many dermatologists transition patients to:
- Non-steroidal topicals like tacrolimus (Protopic) or pimecrolimus (Elidel)
- Phototherapy (UVB light treatments)
- Systemic medications like methotrexate or biologics for severe cases
- Consistent use of fragrance-free moisturizers with ceramides, cholesterol, and fatty acids
Some patients benefit from a "steroid holiday"-a few weeks off steroids, followed by a return to a gentler regimen. This helps reset the skin’s natural balance.
The science behind halobetasol is clear: it’s one of the most potent tools we have to silence severe skin inflammation. But its power demands respect. Used right, it can change a patient’s life. Used wrong, it can leave lasting damage. That’s why it’s not just a cream-it’s a medical decision.
Is halobetasol the same as clobetasol?
Halobetasol and clobetasol are both Class I topical steroids and very similar in strength. Halobetasol is slightly more potent in lab tests, but in practice, dermatologists treat them as interchangeable for most conditions. The choice often comes down to formulation-cream, ointment, or foam-and patient preference.
Can I use halobetasol on my face?
No, unless specifically directed by a dermatologist for a very short time. The skin on your face is thin and sensitive. Halobetasol can cause permanent damage like skin atrophy, visible blood vessels, or steroid-induced acne. Even a few days of use can cause problems here.
How long does halobetasol stay in your system?
Topical halobetasol doesn’t circulate widely in the bloodstream when used correctly. Most of it stays in the skin. But if you use too much, cover it with bandages, or apply it to large areas, some can be absorbed. It has a half-life of about 2-3 hours in the blood, but its effects on skin cells last much longer-up to 72 hours after application.
Can halobetasol cause weight gain or mood changes?
Unlikely with normal use. Systemic side effects like weight gain, mood swings, or high blood pressure happen only with long-term, high-dose use-especially if applied to large areas or under occlusion. For most people using it as directed on small patches, these effects are extremely rare.
Is halobetasol safe for children?
It’s generally not recommended for children under 12. Their skin absorbs more medication, and their adrenal glands are more vulnerable to suppression. In rare, severe cases, a pediatric dermatologist may prescribe it for a very short time with strict monitoring.
Halobetasol’s mechanism is fascinating-binding to glucocorticoid receptors to suppress cytokine transcription is a precise molecular intervention, not just "anti-inflammatory" hand-waving. The gene-level silencing is why it works faster than weaker steroids, but also why rebound flares occur: the immune system hasn’t been trained to self-regulate, only suppressed.
Long-term use isn’t laziness-it’s a failure of the medical system to provide alternatives. We need better access to calcineurin inhibitors and phototherapy, not just stronger steroids.
Also, the skin barrier dysfunction point is critical. Steroids treat symptoms; they don’t repair the lipid matrix. That’s why ceramide moisturizers aren’t optional-they’re foundational.
And yes, Class I means Class I: no face, no groin, no kids under 12 without pediatric dermatology oversight. This isn’t hydrocortisone with a fancy label.
Finally, the 24–48 hour response time? That’s the red flag. If it works too fast, it’s too dangerous to use casually. Respect the potency, or pay the price in striae and adrenal suppression.
Oh please. This is why America’s healthcare is broken. You give someone a steroid that works in two days and suddenly they think it’s a cure-all? No-it’s a chemical muzzle. The real problem? Doctors don’t have time to teach patients how to wean off. They just write the script and move on.
And now we’ve got people using this on their faces like it’s moisturizer. Next thing you know, they’ll be asking for IV steroids for acne. This isn’t medicine-it’s a quick fix culture run amok.
Meanwhile, in Germany, they use light therapy first. In Japan, they use traditional botanicals. But here? Steroid blitzkrieg. That’s not science. That’s convenience.
Thank you for this detailed breakdown-it’s rare to see a post that explains the molecular action without oversimplifying. I’d like to emphasize the importance of formulation: ointments enhance penetration, creams reduce it, and foams are ideal for hairy areas like the scalp. The vehicle matters as much as the dose.
Also, patients often don’t realize that even small amounts applied daily for weeks can cause atrophy. A pea-sized amount for the entire hand is sufficient. Most use way too much.
And yes-tapering isn’t optional. Switching to tacrolimus after 10–14 days reduces rebound risk by over 60% in clinical studies. This isn’t anecdotal; it’s evidence-based practice.
Finally, moisturizers with ceramides, cholesterol, and free fatty acids in a 3:1:1 ratio are the gold standard for barrier repair. Don’t just use any lotion. Use one with the right lipid profile.
Let’s be real: halobetasol is the steroid equivalent of a sniper rifle. You don’t bring it to a skirmish-you use it when the enemy is entrenched in your backyard. But here’s the twist: the pharmaceutical industry doesn’t want you to know that non-steroidal options exist because they’re not profitable. Tacrolimus? Expensive. Phototherapy? Requires equipment. But a $15 tube of halobetasol? That’s a cash cow.
And let’s not pretend the rebound effect is just "immune overcompensation." It’s the body screaming after being gagged for two weeks. You don’t silence a riot and expect silence afterward-you get a massacre.
Also, anyone who uses this on their eyelids deserves what they get. Skin there is 10x thinner than on the forearm. That’s not negligence-it’s ignorance with consequences.
Yeh so I used this stuff on me elbow for psoriasis and it worked like magic but then I stopped and it came back worse so I went back to doc and they said "oh you need to taper" but no one ever told me that before
And now I use this cream with ceramides and it’s okay but I’m scared to ever use halobetasol again cause I don’t trust the system anymore
Also my cousin in Dublin used it on her face and now she looks like a wrinkled old lady at 32 so yeah don’t do it
Interesting how everyone treats halobetasol like it’s some kind of villain. It’s not evil-it’s a tool. A very powerful one. Like a chainsaw. You don’t use it to trim hedges, and you don’t use it without safety gear. But if you’ve got a 6-inch thick psoriatic plaque on your knee that’s been there for a year? This is the only thing that’ll clear it in 10 days.
The problem isn’t the drug. It’s the lack of education. Patients aren’t told how to use it. They’re not told how to stop it. And they’re not told what comes next.
So they panic when their skin flares again. And they blame the steroid. But the steroid didn’t fail. The follow-up plan did.
Maybe we should start labeling these prescriptions with a 3-step guide: 1. Use for 10–14 days. 2. Switch to non-steroidal. 3. Moisturize daily. That’s it. Simple. Effective.
So I read this whole thing and I’m just wondering-how many people actually die from this? Like, is it really that dangerous? I mean, I’ve seen people use it for months and they’re fine. Maybe the doctors are just being extra cautious because they’re scared of lawsuits.
Also, I used it on my scalp for two months and my hair grew back thicker. Maybe it’s not all bad? Maybe the side effects are exaggerated by people who don’t know how to use it properly?
And why is everyone so scared of the word "steroid"? It’s not anabolic. It’s not testosterone. It’s just a molecule that tells your immune system to chill out. What’s the big deal?
As someone who grew up in a household where topical steroids were treated like medicine, not magic, I appreciate the clarity here. In many cultures-especially in parts of Asia and Africa-topical steroids are sold over the counter, and misuse is rampant. I’ve seen children with severe skin atrophy from daily use on their faces.
It’s not just a Western issue. It’s a global public health blind spot. We teach people how to take antibiotics, but not how to use steroids. That’s a failure of medical literacy.
Perhaps the solution isn’t just better prescribing-it’s better patient education. Brochures in clinics, videos on YouTube in multiple languages, community health worker outreach. This drug saves lives-but only when used correctly.
There’s a quiet tragedy here: people who finally find relief after years of suffering, then become terrified of the very thing that gave them back their life.
I used halobetasol for two weeks and my skin looked like it did when I was 12. No itching. No bleeding. No shame.
But then I read the side effects. And now I’m afraid to use it again-even though I know I’ll need it. It’s like being saved from drowning, then being told the life jacket is toxic.
Why can’t we have a middle ground? A safe way to use it without fear? Why is the alternative always "never again" or "forever"?
Maybe the answer isn’t in the drug-but in how we talk about it.
Let me tell you what I wish every patient knew: halobetasol doesn’t cure psoriasis or eczema. It buys you time. Time to rebuild your barrier. Time to find your triggers. Time to try light therapy or biologics without the constant itching screaming in your ears.
Think of it like a fire extinguisher. You don’t live in a house with a fire extinguisher on every wall because you want fires. You keep it because you know fires happen-and you want to be ready.
And yes, moisturizers with ceramides? Non-negotiable. Your skin isn’t just a canvas-it’s a living, breathing, lipid-rich fortress. Steroids tear it down. Moisturizers rebuild it. You need both.
Don’t fear the steroid. Fear the silence after it’s gone.
Just wanted to add: if you’re using halobetasol and your skin starts looking shiny or translucent, stop immediately. That’s not "improvement"-that’s skin atrophy. It’s not reversible. Once the dermis thins, it doesn’t come back.
Also, don’t use it under plastic wrap unless you’re under direct supervision. I’ve seen cases where people wrapped their legs in saran wrap for "better absorption" and ended up with systemic steroid toxicity-adrenal shutdown, electrolyte imbalance, the whole nightmare.
And yes, the rebound effect is real. But it’s not addiction. It’s physiology. Your body forgot how to regulate inflammation because it was told to shut up for two weeks. Now it’s yelling at the top of its lungs.
So taper. Use calcineurin inhibitors. Moisturize. Don’t just quit cold turkey. Your skin will thank you.
Who says this stuff is even safe? Did you know the FDA approved it based on a 12-week study with 87 people? And now it’s being used by millions? Meanwhile, the real cause of psoriasis is gut dysbiosis and mold exposure and no one wants to talk about it because Big Pharma doesn’t sell probiotics for $50 a tube
Also I read somewhere that steroids cause cancer but they cover it up because they make too much money
My cousin’s neighbor’s dog got skin issues and they used this cream and now the dog has three legs and no tail so yeah maybe it’s not all it’s cracked up to be
Also I think the moon landing was faked and halobetasol is part of the plan
Wow. Someone actually wrote a responsible post about steroids. Who’d have thought?
Most of you are still treating this like a miracle cream. It’s not. It’s a chemical scalpel. And if you’re using it without a plan for what comes after, you’re not treating your skin-you’re abusing it.
And if you think moisturizer is just "nice to have," you’re the reason dermatologists have nightmares.
Also, anyone who says "I used it on my face and it worked" is either lying or has a dermatologist on speed dial. Probably both.
That last comment? That’s exactly it. We treat steroids like they’re candy because we don’t understand their weight. They’re not just chemicals-they’re signals. And when you silence the immune system for too long, it doesn’t forget. It waits. And when it comes back? It doesn’t whisper. It roars.
I’m not saying don’t use halobetasol. I’m saying: use it like you mean it. Then let it go. And then-listen to your skin. Not the internet. Not the ad. Not the friend who "swears by it."
Listen. It’s talking.