Tetracycline for Treating Nocardiosis: What You Need to Know

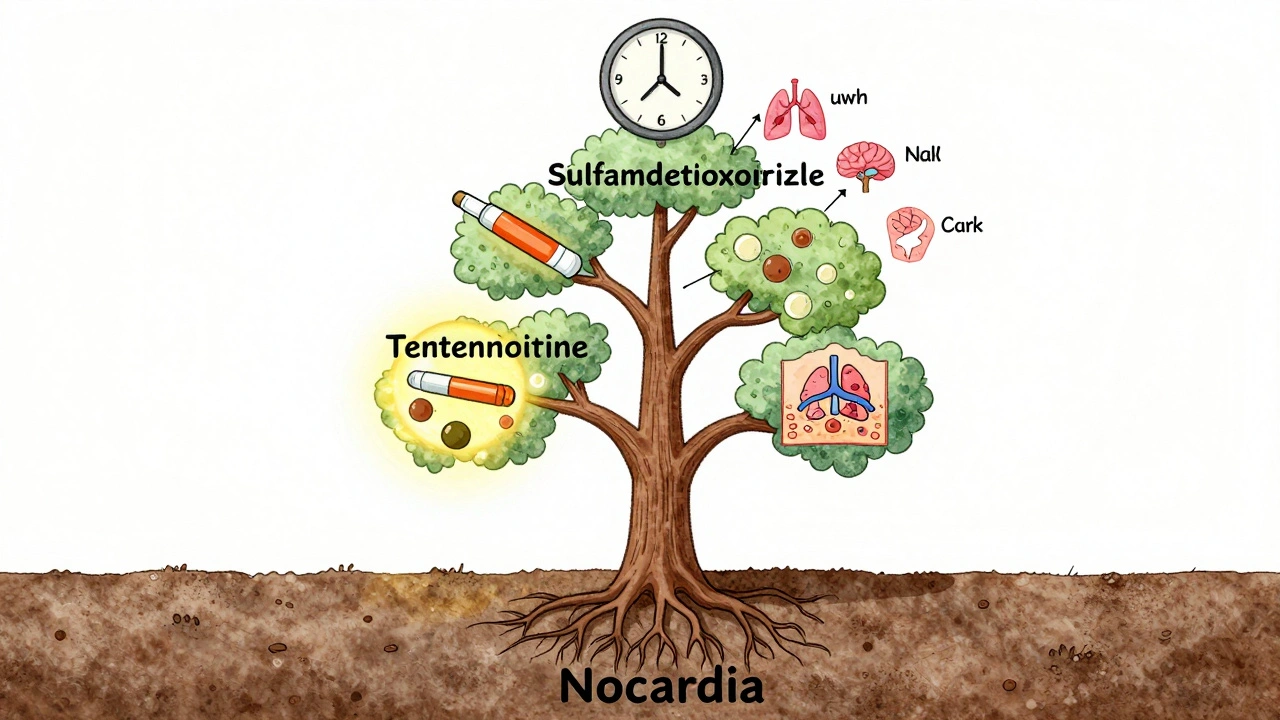
Tetracycline is one of the older antibiotics still used today - and in rare but serious infections like nocardiosis, it can be a lifesaver. Nocardiosis is caused by bacteria from the Nocardia genus, often found in soil and dust. It doesn’t spread from person to person, but when inhaled or introduced through open wounds, it can cause lung infections, brain abscesses, or skin ulcers - especially in people with weakened immune systems. While trimethoprim-sulfamethoxazole is the first-line treatment, tetracycline plays a critical role when patients can’t tolerate the standard drug or when the infection is resistant.
Why Tetracycline Works Against Nocardiosis
Nocardia bacteria are aerobic, gram-positive, and partially acid-fast. They’re not easy to kill. Many antibiotics fail against them because of their thick cell walls and ability to hide inside immune cells. Tetracycline works by blocking protein production in bacteria. It slips into the bacterial ribosome and stops them from building the proteins they need to survive and multiply. This makes it bacteriostatic - it doesn’t kill the bacteria outright, but it stops them from growing, giving your immune system time to clear the infection.
Studies from the Journal of Clinical Infectious Diseases show that tetracycline has in vitro activity against over 70% of Nocardia asteroides strains, which is the most common cause of human infection. In clinical cases where patients couldn’t take sulfa drugs due to allergies or kidney issues, tetracycline was successfully used as a primary or alternative therapy. It’s not always the first choice, but it’s a reliable backup when others fail.
Who Gets Nocardiosis - and Why Tetracycline Might Be Chosen
Nocardiosis mostly affects people with weakened immune systems. This includes:
- People on long-term corticosteroids
- Organ transplant recipients
- Those with uncontrolled HIV/AIDS
- Patients with blood cancers like leukemia
- Individuals with chronic lung diseases like COPD
For these patients, sulfa drugs like trimethoprim-sulfamethoxazole can cause severe side effects - rashes, kidney damage, or bone marrow suppression. When that happens, doctors turn to alternatives. Tetracycline is one of them. It’s also used when the infection is mild to moderate and limited to the lungs, especially if the patient has no history of liver disease or recent antibiotic use.
In one 2023 case series from the Mayo Clinic, five patients with pulmonary nocardiosis who couldn’t take sulfa drugs were treated with doxycycline (a type of tetracycline). All showed clinical improvement within three weeks, and three had complete resolution of lung lesions on follow-up CT scans. The average treatment duration was 11 weeks.
Dosage and How It’s Given
For nocardiosis, tetracycline is usually given orally. The typical adult dose is 500 milligrams every six hours - that’s four times a day. Some doctors prefer doxycycline instead because it’s easier to take: 100 milligrams twice daily. Doxycycline has better absorption, stays in the body longer, and doesn’t need to be taken on an empty stomach like older tetracycline.
Treatment usually lasts at least six months. For brain infections or disseminated disease, treatment can go on for a year or more. Stopping too early is one of the biggest reasons infections come back. Even if symptoms disappear after a few weeks, the bacteria can still be hiding in deep tissues.
It’s important to take tetracycline on an empty stomach - one hour before or two hours after meals. Food, dairy, calcium supplements, and antacids can bind to it and block absorption. You also shouldn’t lie down for at least 30 minutes after taking it to avoid irritation of the esophagus.

Side Effects and Risks
Tetracycline isn’t harmless. Common side effects include:
- Upset stomach, nausea, or diarrhea
- Increased sun sensitivity - you can burn easily
- Yeast infections in the mouth or vagina
- Discoloration of teeth in children under 8
It’s not given to pregnant women or young children because it can permanently stain developing teeth and affect bone growth. It can also cause liver toxicity in rare cases, especially at high doses or in people with pre-existing liver disease.
Drug interactions are another concern. Tetracycline reduces the effectiveness of birth control pills. It can also interact with blood thinners, isotretinoin, and some seizure medications. Always tell your doctor what else you’re taking.
When Tetracycline Isn’t Enough
Not all Nocardia strains respond to tetracycline. Some are naturally resistant. That’s why doctors often start with a broad-spectrum antibiotic and then switch based on lab results. A culture and sensitivity test from a sputum sample, biopsy, or abscess fluid is essential. If the bacteria show resistance to tetracycline, other options include:
- Amikacin (given by IV)
- Ceftriaxone or imipenem
- Linezolid or minocycline (a stronger tetracycline derivative)
Minocycline, in particular, has better penetration into the brain and is often preferred for central nervous system infections. In severe cases, combination therapy - like amikacin plus trimethoprim-sulfamethoxazole or minocycline - is used to increase effectiveness.
Monitoring Treatment Success
How do you know if tetracycline is working? It’s not always obvious right away. Symptoms like cough, fever, or headaches may improve within days, but imaging tests are the real measure. Doctors will repeat chest X-rays or CT scans every 4 to 8 weeks to check if lung nodules or abscesses are shrinking. For brain infections, MRI scans track changes in lesion size.
Blood tests may also be used to monitor liver and kidney function, especially since tetracycline can stress these organs. If your creatinine levels rise or your liver enzymes spike, your doctor may switch you to another antibiotic.
Even after symptoms disappear, follow-up is critical. Recurrence rates for nocardiosis can be as high as 20% if treatment is stopped too soon. Most guidelines recommend continuing antibiotics for at least 3 months after all signs of infection are gone - and longer if the immune system remains compromised.
What to Do If You’re Prescribed Tetracycline
If your doctor prescribes tetracycline for nocardiosis, here’s what you should do:
- Take it exactly as directed - no skipping doses.
- Avoid dairy, calcium, iron, or antacids within two hours of taking it.
- Use sunscreen and avoid prolonged sun exposure.
- Report any unusual rash, yellowing of skin, or severe diarrhea immediately.
- Keep all follow-up appointments for scans and lab work.
- Don’t stop the medication just because you feel better.
Keep a log of your symptoms and side effects. That information helps your doctor adjust your treatment if needed.
Alternatives to Tetracycline
While tetracycline is useful, it’s not the only option. Here’s how it compares to other drugs used for nocardiosis:
| Antibiotic | Route | Typical Dose | Pros | Cons |
|---|---|---|---|---|
| Trimethoprim-sulfamethoxazole | Oral/IV | 15 mg/kg/day | First-line; high efficacy | Allergy risk; kidney/liver toxicity |
| Tetracycline | Oral | 500 mg 4x/day | Good for sulfa-allergic patients; affordable | Multiple daily doses; food interactions |
| Doxycycline | Oral | 100 mg 2x/day | Easier dosing; better absorption | Still requires fasting; sun sensitivity |
| Minocycline | Oral | 100 mg 2x/day | Best brain penetration; longer half-life | Higher risk of dizziness; rare autoimmune reactions |
| Amikacin | IV | 15 mg/kg/day | Strong for severe cases | Requires hospitalization; kidney/ear damage risk |
For most patients, the choice comes down to tolerance, infection location, and immune status. Tetracycline remains a practical option when other drugs aren’t safe.
Final Thoughts
Nocardiosis is rare but dangerous. Left untreated, it can be fatal - especially in immunocompromised people. Tetracycline isn’t flashy, but it’s proven. It’s been around since the 1940s, and in the right cases, it still saves lives. The key is using it correctly: the right dose, the right duration, and with full awareness of its limits and risks.
If you’re on tetracycline for nocardiosis, patience and discipline matter more than anything. This isn’t a two-week fix. It’s a long haul - but with the right approach, recovery is possible.
Can tetracycline cure nocardiosis completely?
Yes, tetracycline can cure nocardiosis, but only if taken correctly and for the full course - often 6 to 12 months. Stopping early increases the risk of relapse. Cure depends on the infection’s severity, the patient’s immune status, and whether the bacteria are sensitive to the drug.
Is tetracycline better than sulfa drugs for nocardiosis?
No, sulfa drugs like trimethoprim-sulfamethoxazole are more effective and are the first-line treatment. Tetracycline is used only when sulfa drugs can’t be taken due to allergies or side effects. It’s a backup, not a replacement.
How long does it take for tetracycline to start working on nocardiosis?
Symptoms like fever or cough may improve within 1 to 2 weeks, but the bacteria take much longer to clear. Imaging tests show improvement over months. Treatment lasts at least 6 months, even if you feel fine sooner.
Can I take tetracycline with food?
No. Tetracycline should be taken on an empty stomach - at least one hour before or two hours after eating. Dairy, calcium, iron, and antacids block its absorption. Doxycycline is more forgiving, but classic tetracycline requires strict timing.
What happens if I miss a dose of tetracycline?
If you miss a dose, take it as soon as you remember - unless it’s almost time for the next one. Never double up. Missing doses can let the bacteria grow back and lead to resistance. If you miss more than one dose, contact your doctor.
Is tetracycline safe for elderly patients?
It can be, but with caution. Older adults are more prone to kidney and liver issues, which can affect how tetracycline is processed. Doctors often lower the dose or choose doxycycline instead. Liver function tests are usually monitored during treatment.
Bro this post is fire. Tetracycline for nocardiosis? I had a cousin in Delhi who got hit with this after working in a construction site. Docs threw sulfa at him, he broke out in rashes like a horror movie. Switched to doxycycline and he’s been fine for 3 years now. No jokes - this stuff saves lives when the big guns fail.
Man. I’ve seen this play out in the ER more than once. Tetracycline isn’t glamorous, but it’s like that one friend who shows up when everyone else ghosts. Quiet. Reliable. Doesn’t brag. Just does the job. And yeah - the fasting thing? Brutal. But if you wanna live, you learn to love the empty stomach.
It is a matter of considerable clinical significance that tetracycline, a compound first synthesized in the mid-twentieth century, retains demonstrable efficacy against Nocardia asteroides despite the advent of newer antimicrobial agents. The persistence of its utility underscores the evolutionary resilience of certain bacterial targets and the inadequacy of our current paradigm in antibiotic innovation.
Wait so you’re telling me I have to take this stuff on an empty stomach and not lie down for 30 minutes?? I’m already on 7 meds and I forget to drink water sometimes 😭 I just want to feel better without feeling like I’m in a military boot camp for bacteria. Why can’t medicine be easier??
How quaint. Tetracycline? In 2024? I suppose the pharmaceutical industry still clings to its 1940s nostalgia like a relic of colonial medicine. The real breakthroughs lie in targeted phage therapy and AI-driven antimicrobial design - not rehashing antibiotics that make your teeth turn gray. This post reads like a textbook from a forgotten era.
Just wanted to add - if you’re on doxycycline and you forget to take it before breakfast, don’t panic. Just take it later with a light snack. The rules aren’t always black and white. I’ve seen patients do fine even with minor slip-ups. Just don’t make a habit of it. And yeah - sunscreen. Always. Sunburns are no joke.
Let me tell you something - this isn’t just about antibiotics. This is about discipline. Nocardiosis doesn’t care how smart you are or how rich you are. It only cares if you show up. Take your pills. Don’t skip. Don’t stop because you feel better. Your immune system is your teammate - but it needs you to do your part. This treatment is a marathon, not a sprint. And trust me - the finish line is worth it.
Everyone’s acting like tetracycline is some miracle drug. Newsflash - it’s bacteriostatic, not bactericidal. That means it just puts the bacteria to sleep, doesn’t kill ‘em. Meanwhile, amikacin? That’s a sledgehammer. And minocycline? Way better brain penetration. Why are we still talking about this 70-year-old drug like it’s the only option? Lazy medicine.
Just got prescribed doxycycline for this 😅 thanks for the heads up on the sun thing - I’m already looking like a lobster after 10 minutes outside. 🌞🩹 Also, side note: I bought a little pill organizer with 4 slots. Life changed. 🙌
So like… if I just stop after 3 months because I’m tired of taking pills, what’s the worst that could happen? I mean I feel fine now right? Like come on. I’m not a robot. 🤷♂️
Interesting
When I was working in infectious disease at Johns Hopkins, I saw a patient who had been on tetracycline for 14 months after a brain abscess from Nocardia. He was a retired teacher, immunocompromised from a bone marrow transplant, and he took every single pill on time, even when he was too nauseous to eat. He’d write notes in a little journal: Day 127 - no fever. Day 189 - CT scan showed 40% reduction. He didn’t just survive - he thrived. And it wasn’t because of magic. It was because he showed up. Every single day. That’s the real story here. Not the drug. Not the dose. The human will to keep going when everything says stop.