Systemic Antifungals and Statins: What You Need to Know About Dangerous Drug Interactions
When you’re on a statin to lower cholesterol or an immunosuppressant after a transplant, adding an antifungal might seem like a simple fix for a fungal infection. But here’s the hard truth: some antifungals can turn your safe medications into a ticking time bomb. The real danger isn’t the infection-it’s what happens when these drugs collide inside your body.
Why Azole Antifungals Are the Problem
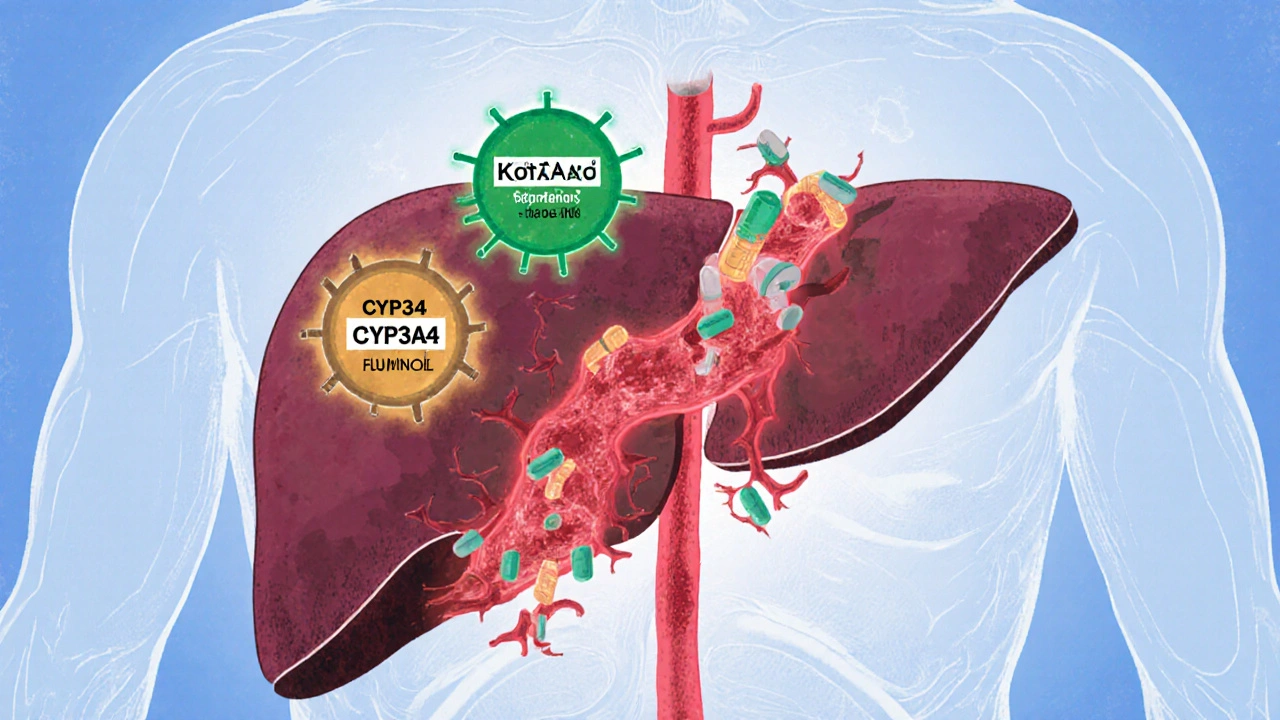
Not all antifungals are created equal. The azole class-drugs like fluconazole, itraconazole, voriconazole, posaconazole, and ketoconazole-are the most common systemic antifungals used for serious fungal infections. They work by blocking a fungal enzyme called lanosterol 14-alpha-demethylase. But here’s the catch: that same enzyme exists in your liver, and it’s part of a family called cytochrome P450 (CYP). These enzymes don’t just fight fungi-they break down your statins, immunosuppressants, and dozens of other drugs. Azoles, especially the strong ones like ketoconazole and posaconazole, shut down CYP3A4, the most important enzyme in your liver for drug metabolism. It handles about 30% of all medications you take. When it’s blocked, your body can’t clear statins or immunosuppressants properly. That means those drugs build up to dangerous levels in your blood.Statins at Risk: Which Ones Are Most Dangerous?
Not all statins are equally risky. If you’re taking simvastatin, lovastatin, or atorvastatin, you’re in the highest-risk group. These are metabolized almost entirely by CYP3A4. When an azole antifungal is added, their blood levels can spike 10 to 20 times higher than normal. That’s not a small increase-it’s a medical emergency waiting to happen. The result? Statin-associated myopathy. At first, it’s just muscle pain or weakness. But it can quickly turn into rhabdomyolysis, a condition where muscle cells break down and flood your bloodstream with toxic proteins. This can cause kidney failure, heart rhythm problems, and even death. Studies show the risk of rhabdomyolysis increases tenfold when statins are taken with CYP3A4 inhibitors like azoles. Pravastatin and rosuvastatin are safer choices. They don’t rely heavily on CYP3A4 for breakdown. But even they aren’t risk-free. Ketoconazole also blocks the OATP1B1 transporter, which helps move these statins out of the liver. So even “safer” statins can pile up if you’re on ketoconazole.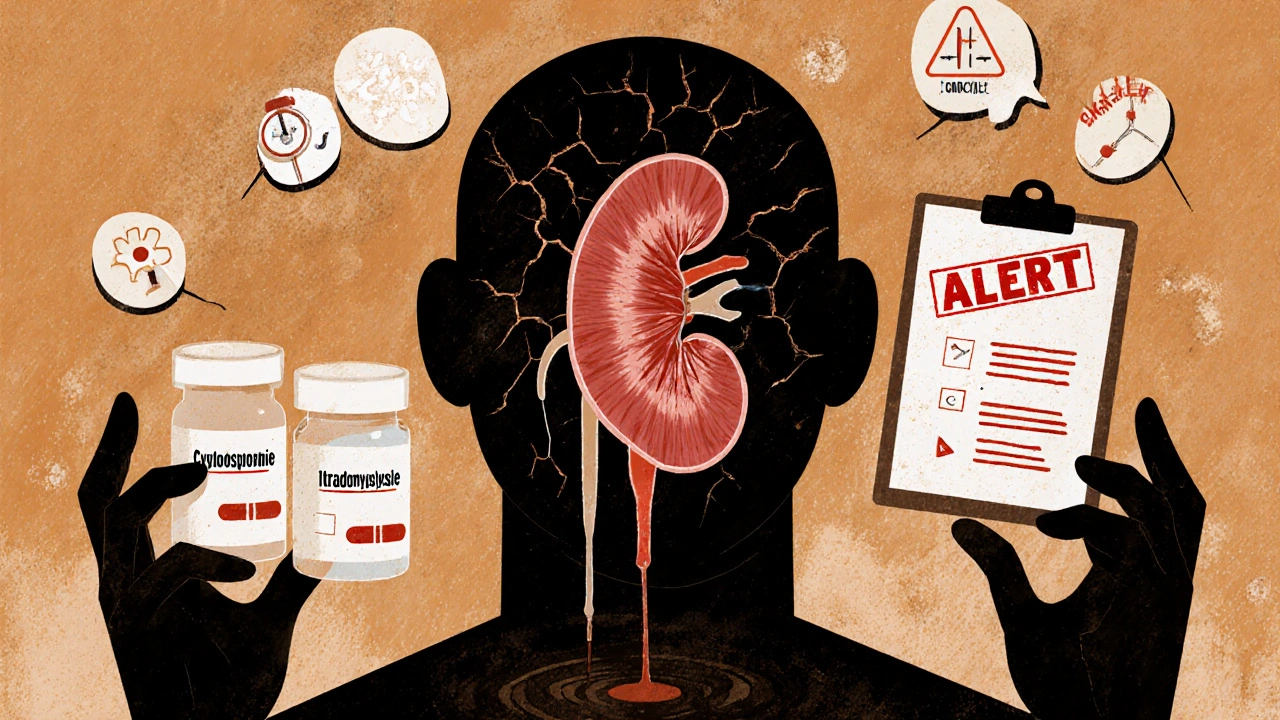
Immunosuppressants: A Double Whammy
If you’ve had a kidney, liver, or heart transplant, you’re likely on cyclosporine, tacrolimus, sirolimus, or everolimus. These drugs are lifesavers-but they’re also CYP3A4 inhibitors themselves. That means they already slow down how fast your body clears statins. Add an azole antifungal on top? You’re stacking two powerful inhibitors together. In transplant patients, studies show statin levels can jump 3 to 20 times higher when combined with cyclosporine alone. Add fluconazole or itraconazole? That number climbs even more. The risk of muscle damage in this group hits 25%-far higher than in the general population. And when creatine kinase (CK) levels exceed 10,000 U/L, you’re looking at full-blown rhabdomyolysis. Many of these cases are preventable.What to Do If You Need an Antifungal
If you’re on a statin and need an antifungal, don’t panic-but don’t ignore it either. Here’s what actually works:- Stop simvastatin, lovastatin, and atorvastatin completely while taking ketoconazole, itraconazole, or posaconazole. Restart them only after the antifungal is fully cleared-this can take days to weeks, especially with posaconazole, which has a half-life of 24-30 hours.
- Switch to pravastatin or rosuvastatin if you need ongoing cholesterol control. Use the lowest effective dose: 10-40 mg daily for pravastatin, 5-20 mg daily for rosuvastatin.
- Avoid fluconazole if possible for high-risk patients. While it’s weaker than ketoconazole, it still inhibits CYP2C19 and CYP3A4. Use it only if no other option exists.
- For transplant patients, your doctor should monitor your immunosuppressant blood levels closely. When you start an azole, they’ll likely lower your cyclosporine or tacrolimus dose by 30-50% to avoid toxicity.
- Never take simvastatin above 10 mg daily if you’re on a moderate CYP3A4 inhibitor like fluconazole or diltiazem.
What About Newer Antifungals?
There’s some good news. Newer drugs like isavuconazole are weaker CYP3A4 inhibitors and don’t require full statin discontinuation in many cases. And olorofim, still in trials, works through a completely different pathway-no CYP450 involvement at all. That means it could be a game-changer for patients on multiple medications. But here’s the reality: most doctors still reach for fluconazole or itraconazole because they’re cheaper and more familiar. And pharmacies still dispense them without checking for interactions. That’s why the American Society of Health-System Pharmacists created a protocol requiring pharmacists to verify statin-azole combinations before dispensing. In hospitals using this system, dangerous pairings dropped by 63%.What You Can Do Right Now
You don’t need to be a doctor to protect yourself. Here’s what to do:- Know your meds. If you’re on a statin or immunosuppressant, ask your pharmacist: “Is this antifungal safe with what I’m already taking?”
- Keep a list. Write down every medication you take, including over-the-counter drugs and supplements. Bring it to every appointment.
- Watch for symptoms. Muscle pain, weakness, dark urine, or unexplained fatigue aren’t normal. Call your doctor immediately if you feel them.
- Ask about alternatives. Is there a topical antifungal you can use instead? Could a different statin work? Don’t assume the first option is the only one.
These interactions aren’t rare. They happen every day in clinics and hospitals. In 2012, researchers found that even with clear warnings on drug labels, doctors still prescribed dangerous combinations regularly. The problem isn’t ignorance-it’s habit, pressure, and lack of communication.
But you have power. You’re the one who takes the pills. You’re the one who notices when something feels off. Speak up. Ask questions. Push for safer options. Your muscles, your kidneys, and your life depend on it.
Can I take fluconazole with my statin?
It depends. Fluconazole is a moderate CYP3A4 inhibitor and also blocks CYP2C19. It’s safer than ketoconazole or itraconazole, but still risky with simvastatin, lovastatin, or atorvastatin. If you’re on one of those, avoid fluconazole. If you’re on pravastatin or rosuvastatin, it’s usually okay at low doses-but your doctor should still monitor you. Never take fluconazole with simvastatin above 10 mg daily.
What are the signs of rhabdomyolysis?
Rhabdomyolysis starts with muscle pain, tenderness, or weakness-often in the shoulders, thighs, or lower back. You might feel unusually tired or notice dark, tea-colored urine. In severe cases, you may have nausea, vomiting, or confusion. If you have any of these symptoms while on statins and antifungals, stop the meds and get medical help immediately. A simple blood test for creatine kinase (CK) can confirm muscle breakdown.
Why can’t I just lower my statin dose instead of stopping it?
Lowering the dose helps, but it’s not enough. When CYP3A4 is blocked, even a small amount of statin can build up to toxic levels. For example, 20 mg of simvastatin with ketoconazole can act like 200-400 mg in your bloodstream. That’s why guidelines say to stop simvastatin, lovastatin, and atorvastatin completely during azole therapy. Switching to pravastatin or rosuvastatin is the only safe way to keep cholesterol under control.
I’m on cyclosporine after a transplant. Can I still take a statin?
Yes, but with extreme caution. Cyclosporine alone increases statin levels by 3-20 times. Adding an azole antifungal makes it worse. Your doctor should use the lowest possible statin dose-usually pravastatin 10 mg or rosuvastatin 5 mg daily. They’ll also monitor your creatine kinase and kidney function weekly during antifungal treatment. Never start or stop any of these drugs without medical supervision.
Are there any natural alternatives to systemic antifungals?
For mild fungal infections like athlete’s foot or yeast infections, topical antifungals (creams, sprays, or powders) are often enough and carry no interaction risk. But for systemic infections-like fungal pneumonia, bloodstream infections, or deep tissue infections-topical treatments won’t work. There are no proven natural alternatives that can replace systemic antifungals in serious cases. Skipping treatment can be life-threatening. Always follow your doctor’s advice for serious infections.
Just got prescribed fluconazole yesterday and I’m on rosuvastatin-glad I checked this thread first. My pharmacist didn’t mention a thing.
Let’s be clear: this isn’t a ‘drug interaction’-it’s a systemic failure of pharmaceutical oversight. The CYP3A4 enzyme isn’t just ‘inhibited’-it’s criminally neglected in medical education. We’ve known since the 1990s that azoles and statins are a lethal cocktail, yet pharmacies still dispense them like candy. The FDA’s warning labels? A joke. They’re buried in 47-point font on page 12 of a 200-page insert. Meanwhile, patients are dying because doctors are too lazy to open their electronic health records. This isn’t negligence-it’s institutional malpractice.
And don’t get me started on ‘natural alternatives.’ You can’t cure systemic candidiasis with garlic and yogurt. That’s not medicine-it’s spiritual bypassing disguised as wellness. If you have a fungal infection in your bloodstream, you need pharmacology-not a juice cleanse.
Pravastatin and rosuvastatin aren’t ‘safer’-they’re merely less likely to kill you instantly. But even they’re not immune to OATP1B1 blockade. Ketoconazole? It’s a molecular wrecking ball. It doesn’t just inhibit-it obliterates. And yet, it’s still in use because it’s cheap. Profit over patient safety. Again.
The fact that ASHP had to create a mandatory protocol to stop this carnage says everything. Hospitals that implemented it saw a 63% drop. So why isn’t it federal law? Why are we still relying on pharmacists to be the last line of defense? Because the system doesn’t care until someone dies. And then? A press release. A footnote. A quiet update to the formulary. And the cycle continues.
You want to protect yourself? Don’t rely on your doctor. Don’t rely on your pharmacist. Print this out. Highlight every line. Bring it to every appointment. Ask: ‘What’s the CYP3A4 profile of this drug?’ If they don’t know-fire them. Your muscles aren’t expendable.
Wow. So we’re supposed to believe that a 2012 study showing doctors still prescribe dangerous combos is somehow new info? This is basic pharmacology 101. Why are we even having this conversation in 2025? Also, ‘natural alternatives’? Please. If you’re Googling ‘cure fungal infection with turmeric,’ you shouldn’t be allowed near a pharmacy.
Thank you for this. I’m a nurse and I’ve seen two patients in the last year with rhabdomyolysis from this exact combo. One was on simvastatin and fluconazole-she didn’t know they were dangerous. Her CK was over 50,000. She’s okay now, but barely. Please, if you’re on a statin and get an antifungal script-call your pharmacy before filling it. Ask them to check interactions. It takes 90 seconds. It could save your life.
bro i took ketoconazole with atorvastatin for 3 weeks and i’m still alive lmao 🤡
As someone who’s lived in both the U.S. and India, I’ve seen how differently this plays out. In the U.S., it’s all about liability and labels. In India? It’s about access. Fluconazole is sold over the counter for $0.50. Simvastatin? $1.50. No one’s checking interactions because no one can afford to stop either. I’ve seen grandmas on both drugs, and they’re fine-until they’re not. The real issue isn’t just the science-it’s the inequality. The people who need this info most can’t access it. And when they get sick? They don’t have the luxury of switching statins or waiting weeks for a safer antifungal. This isn’t just a medical problem-it’s a social justice crisis.
I’m on cyclosporine after a kidney transplant and just got prescribed itraconazole for a stubborn nail fungus. My doctor didn’t say anything about my statin, but now I’m terrified. I’m switching to pravastatin tomorrow. I printed this whole thread and brought it to my appointment. I’m not taking chances. This is life or death. Thank you to whoever wrote this-seriously.
Did you know that the FDA approved these drugs knowing the interaction? Big Pharma knows statins are profitable. Antifungals are too. They don’t want you to switch to safer options because they make less money. That’s why they bury the warnings. And now they’re pushing ‘newer antifungals’-but those are 10x more expensive. This isn’t science. It’s a money game. They’re letting people die to keep the cash flowing. You think your doctor’s looking out for you? They’re paid by the system. The system doesn’t want you healthy. It wants you dependent.
Wait-does this apply to topical antifungals too? Like clotrimazole cream for athlete’s foot? I don’t want to overreact, but I’m paranoid now.
Thank you for this comprehensive and meticulously researched post. The clinical implications are profound, and the practical recommendations are both evidence-based and actionable. I have shared this with my entire clinical team, and we are revising our internal protocols to include mandatory pharmacist review for all azole-statin combinations. Patient safety must be non-negotiable. I encourage all readers to print this, keep it in their medication binder, and bring it to every visit. Knowledge is the most powerful tool we have.
I’m on rosuvastatin and just got fluconazole for a yeast infection. My doctor said it’s fine, but now I’m second-guessing everything. Should I still be worried? I’m not having any symptoms yet, but I don’t want to wait until I’m in the ER.