SSRI and SNRI Discontinuation Timelines: What Patients Can Expect

SSRI/SNRI Discontinuation Timeline Calculator
How long will your withdrawal last?
This tool estimates your potential withdrawal timeline based on your medication's half-life and tapering approach.
Stopping SSRIs or SNRIs isn’t as simple as taking your last pill and calling it done. For many, the real challenge begins after the final dose. Withdrawal symptoms don’t mean you’re relapsing-they’re your body adjusting to life without the drug. And if you’re not prepared, those symptoms can feel terrifying: dizziness, brain zaps, nausea, or sudden anxiety that comes out of nowhere. The good news? You can manage this. The key is understanding SSRI discontinuation timelines and how your specific medication behaves in your body.
Why Withdrawal Happens at All
Your brain adapts to antidepressants over time. SSRIs and SNRIs increase serotonin (and sometimes norepinephrine) levels by blocking its reabsorption. After weeks or months, your brain reduces its own production and receptor sensitivity to compensate. When you stop the drug, that balance is thrown off. Your brain hasn’t had time to readjust. That’s when withdrawal symptoms appear. This isn’t addiction. It’s pharmacological adaptation. But the symptoms can be so intense that many people think they’re having a relapse of depression. In fact, studies show about 30% of people who stop too quickly end up going back on medication because they mistake withdrawal for their original illness returning.Half-Life Matters More Than You Think
Not all antidepressants are created equal when it comes to stopping. The half-life-the time it takes for half the drug to leave your system-determines how quickly symptoms hit. Take paroxetine (Paxil). With a 24-hour half-life, symptoms can start within 1-3 days of skipping a dose. Same with sertraline (Zoloft) and escitalopram (Lexapro). These drugs leave your system fast. That means your brain feels the drop quickly. Now look at fluoxetine (Prozac). Its half-life is 4-6 days. That’s longer than most people’s daily routine. Symptoms might not show up for weeks. Some patients don’t notice anything until a month after their last pill. That’s why fluoxetine is often used as a bridge when switching off other SSRIs-it gives your brain more time to adjust. SNRIs like venlafaxine (Effexor) are even trickier. With a 5-hour half-life, symptoms can hit within 24 hours. That’s why venlafaxine withdrawal is often the most severe. Dizziness affects 78% of people. Electric shock sensations-called “brain zaps”-show up in 62%. Nausea? 55%. These aren’t rare side effects. They’re the norm.How Long Should You Taper?
Here’s where things get messy. Clinical guidelines say one thing. Real patients report something else. Many doctors recommend a 2-4 week taper. That’s what’s printed in textbooks. But a 2023 British Medical Journal study found that 68% of people who tapered this fast ended up with severe withdrawal or relapse. Only 22% had smooth exits when tapers lasted over 20 weeks. Meanwhile, patient communities like Reddit’s r/antidepressants (with over 285,000 members) report that 68% of people experience symptoms longer than the 1-2 weeks most doctors promise. One person on Reddit described paroxetine withdrawal lasting 11 months-even after a 6-month taper. The Surviving Antidepressants community found that 73% of members needed over a year to stop safely. A third needed 18 months or more. So what’s the real answer? It’s not one-size-fits-all. The best approach is symptom-driven tapering. If you feel worse after a reduction, pause. Stay at that dose until you stabilize. Then go slower next time. Some people need to drop by 10% of their dose every 4-8 weeks. Others need 1-2.5% drops using liquid formulations.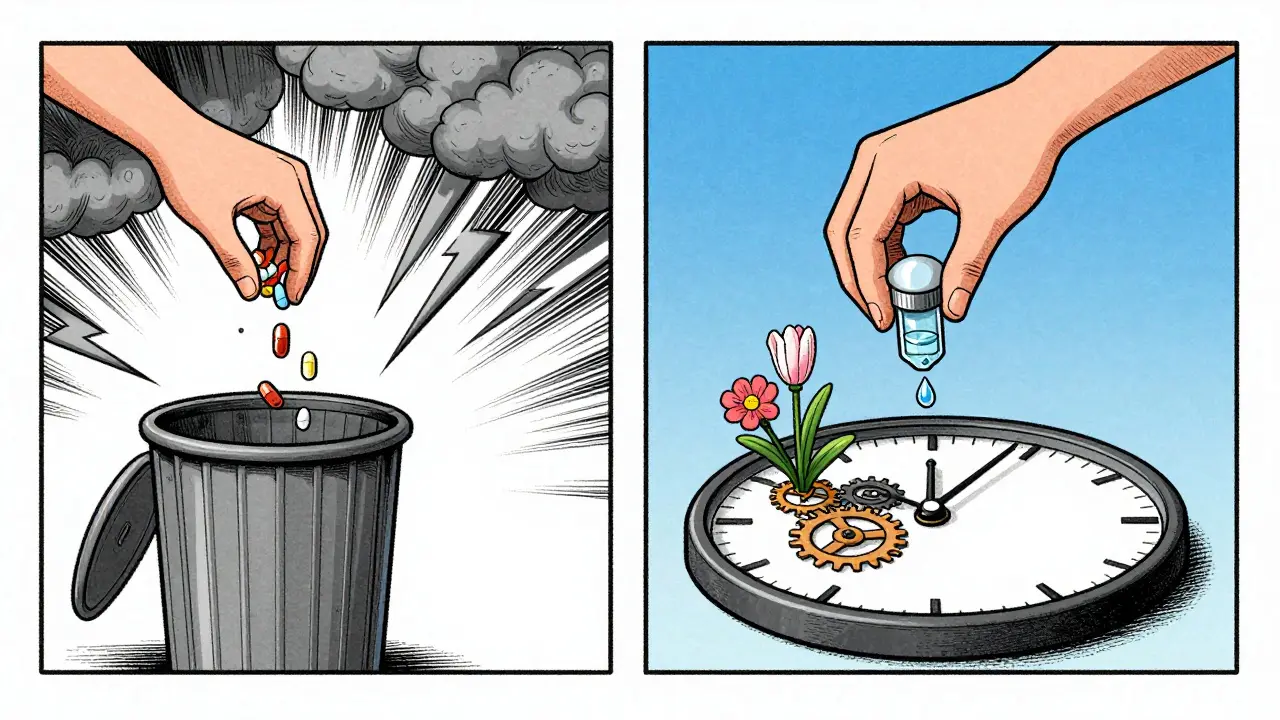
Medication-Specific Tips
Paroxetine (Paxil): One of the hardest to stop. Even small reductions can trigger symptoms. Consider switching to fluoxetine before tapering. It’s easier to manage. Fluoxetine (Prozac): You can taper faster because it lingers in your system. But don’t be fooled-symptoms can appear weeks later. Monitor for at least 3 months after your last dose. Venlafaxine (Effexor): The most aggressive tapering is needed. Never cut more than 10% at a time. Use liquid versions if possible. A 2023 University of Toronto study showed micro-tapers (1-2.5% reductions) cut severe symptoms by 63%. Duloxetine (Cymbalta): Avoid crushing or opening capsules. That changes how the drug releases. Use liquid formulations or switch to another SSRI for tapering. Generic switches: Don’t let your pharmacy switch your brand to a generic without telling you. A 20% concentration difference can mimic abrupt withdrawal. Always ask for the same manufacturer.What Symptoms to Watch For
Symptoms usually start within days of reducing your dose. They peak around day 3-5 and fade in 1-2 weeks for most. But not everyone. Common signs:- Brain zaps (electric shock feelings in the head)
- Dizziness or vertigo
- Nausea, vomiting, or diarrhea
- Insomnia or vivid dreams
- Anxiety or panic attacks
- Flu-like symptoms (fatigue, muscle aches)
- Sensory changes (light sensitivity, tingling)
- Thoughts of self-harm or suicide
- Severe panic attacks that don’t subside
- Confusion, hallucinations, or seizures

What to Do If Symptoms Hit
If you start feeling worse during a taper:- Stop reducing. Stay at your current dose until symptoms fade.
- It usually takes less than 72 hours to feel better after returning to your last stable dose.
- Once stable, try a smaller reduction-maybe half of what you tried before.
- Keep a symptom journal. Note the day, dose, and what you felt. This helps your doctor adjust your plan.
What’s Changing in 2025?
The field is finally catching up to patient experiences. The FDA now requires updated medication guides that include individualized tapering advice based on half-life. The American Psychiatric Association is rolling out new guidelines in 2024 that will include patient-reported outcomes. The European Medicines Agency admitted their current guidelines miss 40-60% of real-world cases. A major NIH-funded study called TAPER-SSRI is tracking 1,200 people through 12-month tapers. Results are due in late 2025. Until then, the best advice is simple: listen to your body. Your symptoms are your guide.Final Thoughts
Stopping SSRIs or SNRIs isn’t about speed. It’s about safety. The goal isn’t to get off the drug as fast as possible. It’s to get off without losing your mind-or your stability. If you’re thinking about stopping, talk to a provider who’s trained in gradual tapering. Ask if they’ve used liquid formulations. Ask if they’ve seen patients through long tapers. Don’t settle for a 2-week plan if you’ve been on the drug for years. You’ve done the hard work getting better. Don’t let a rushed stop undo it.How long do SSRI and SNRI withdrawal symptoms last?
For most people, symptoms last 1-2 weeks. But about 10-20% experience protracted symptoms that last months. Factors like medication half-life, duration of use, and taper speed affect this. Paroxetine and venlafaxine tend to cause longer withdrawal than fluoxetine. Patient surveys show 46% of people need more than 6 months to fully taper without severe symptoms.
Can I stop SSRIs cold turkey?
It’s not recommended. Stopping abruptly increases your risk of severe withdrawal symptoms like brain zaps, dizziness, nausea, and anxiety. For drugs with short half-lives like paroxetine or venlafaxine, symptoms can hit within 24 hours. Even fluoxetine, which has a long half-life, can cause delayed withdrawal. A gradual taper reduces risk and improves success.
Why do some people have worse withdrawal than others?
Several factors play a role. Longer treatment duration (over 6 months) increases risk. Genetic differences affect how your body metabolizes the drug. Some people are more sensitive to serotonin changes. Stopping too fast, switching generics without warning, or having anxiety disorders also raise your risk. Women and older adults tend to report more intense symptoms.
Is it normal to feel worse before feeling better during tapering?
Yes. Withdrawal symptoms often peak within the first week after a dose reduction. That doesn’t mean you’re relapsing-it means your brain is adjusting. If symptoms are mild to moderate, staying at the same dose for 2-4 weeks usually helps them fade. If they’re severe, going back to your last stable dose and tapering slower is the safest move.
Should I switch to fluoxetine before stopping?
For some people, yes. If you’re on a short-half-life SSRI like paroxetine or sertraline, switching to fluoxetine can make tapering smoother. Fluoxetine’s long half-life acts as a buffer, reducing the speed of withdrawal. This is a common strategy used by specialists. But it must be done under medical supervision to avoid serotonin overload.
Are liquid formulations better for tapering?
Yes, especially for drugs like venlafaxine or paroxetine. Liquid forms allow for micro-tapers-reductions as small as 1-2.5%. A 2023 University of Toronto study showed this cut severe symptoms by 63% compared to tablet tapers. If your pharmacy doesn’t offer it, ask your doctor for a prescription. Many compounding pharmacies can make custom liquid doses.
How do I know if it’s withdrawal or a relapse?
Withdrawal symptoms usually come on quickly after a dose change and include physical signs like dizziness, brain zaps, nausea, or electric shock sensations. Relapse symptoms develop slowly and are more emotional-persistent sadness, loss of interest, hopelessness. If symptoms appear within days of reducing your dose, it’s likely withdrawal. If they appear weeks later without a dose change, it could be relapse. A doctor can help you tell the difference.
Can I use supplements to help with withdrawal?
Some people report relief from omega-3s, magnesium, or vitamin B12, but there’s no strong evidence they prevent or cure withdrawal. Don’t rely on supplements alone. The most effective tool is a slow, controlled taper. Always talk to your doctor before adding anything-some supplements can interact with antidepressants or affect serotonin levels.
What if my doctor won’t help me taper slowly?
Many primary care providers aren’t trained in gradual tapering. If your doctor refuses to help, ask for a referral to a psychiatrist or psychopharmacologist. You can also seek support from organizations like Surviving Antidepressants or the Icarus Project. Bring printed guidelines from the Cleveland Clinic or the British Association of Psychopharmacology to your appointment. You’re not asking for something unusual-you’re asking for evidence-based care.
Is it ever too late to start a slow taper?
No. Even if you’ve already stopped and are struggling, you can restart at your last stable dose and begin a slower taper. Many people do this successfully. The goal isn’t to have never stopped-it’s to stop safely. It’s never too late to prioritize your nervous system’s healing.
This is the most balanced, well-researched post I've seen on this topic. Finally, someone gets it. Tapering isn't a race. Your nervous system doesn't care about your calendar.
I made it through 14 months on a 1% monthly taper. It was hell, but I'm finally drug-free and stable.
I'm sorry, but this post is dangerously misleading. You're encouraging people to ignore medical advice and go rogue with liquid tapers! The FDA doesn't endorse micro-dosing! This is how people end up in the ER!
Ugh. Another one of those 'listen to your body' hippie nonsense posts. If your doctor says two weeks, then two weeks it is. You're not a scientist, you're a patient. Do as you're told.
i just wanna say... the brain zaps? they feel like your soul is being unplugged. like your consciousness is glitching. and no one talks about how lonely it is when you're the only one who knows what that feels like.
There's a deeper truth here that society refuses to acknowledge: antidepressants don't fix the root causes of suffering-they silence the signal so we stop listening to the message. Discontinuation isn't just about neurochemistry; it's about reclaiming the raw, unfiltered experience of being human again. The withdrawal isn't the enemy-it's the voice of your nervous system screaming, 'I'm still here!' And maybe that's the real healing.
Prozac is not a magic fix. It's just a longer delay before the crash. Stop romanticizing it.
The fact that you need a 6-month taper means the drug never helped you in the first place. You were just chemically sedated. The system rewards dependency, not recovery.
I am from India and we dont have this problem here. Doctors here just say stop and you stop. No liquid stuff. No brain zaps. Just life. Maybe your culture makes you weak?
I appreciate the depth of this. I was on venlafaxine for 8 years. My taper took 22 months. I used a compounding pharmacy. I kept a journal. I cried a lot. But I made it. And I’m not ashamed of how long it took.
I think the real issue is that we treat mental health like a software update-just uninstall and reinstall. But the mind isn't a machine. It's a living ecosystem. You can't just reset it without consequences.
This post saved my life 🙏 I tapered for 18 months. Used liquid sertraline. My doc was skeptical at first. But I brought the BMJ study. Now she refers others to me. You’re not alone. 💙
This is all just Big Pharma propaganda. They want you to think you need a year to quit so you'll keep buying pills. The real withdrawal is the system keeping you hooked. Trust no one.
half life thing is overrated. its all in your head. i stopped cymbalta in 3 days. fine.
I must insist: this post is not medically sound. The references to Reddit and patient forums are not peer-reviewed. This is anecdotal garbage masquerading as science. You are putting lives at risk.