Specific IgE Testing: How to Identify Allergens and Understand Your Results
What Specific IgE Testing Actually Measures
Specific IgE testing is a blood test that looks for antibodies your body makes in response to particular allergens. These antibodies are called immunoglobulin E, or IgE. When you’re allergic to something-like peanuts, pollen, or cat dander-your immune system overreacts and produces IgE antibodies that target those substances. The test doesn’t tell you if you’re allergic based on symptoms. It tells you if your blood has those specific antibodies, which is a key clue doctors use to confirm an allergy.
Back in the 1970s, this test was called RAST, and it only gave a yes-or-no answer. Today, it’s much more precise. The most common method now is called ImmunoCAP, which uses a 3D polymer capsule to capture IgE antibodies from your blood. The result? A number in kUA/L units. A level below 0.35 kUA/L is considered negative. Anything above that suggests sensitization-but not always a true allergy.
Why This Test Is Done (And When It’s Not)
Doctors don’t order this test just because someone says they feel funny after eating almonds. They order it when there’s a clear pattern: hives after shellfish, wheezing after being around dogs, or anaphylaxis after eating eggs. The test helps confirm if those reactions are IgE-driven.
It’s especially useful when skin testing isn’t possible. If you have severe eczema covering a big part of your skin, or if you’re on antihistamines that can’t be stopped for 3 to 5 days, blood testing is the next best option. In pediatric clinics, about 27% of kids get blood tests instead of skin pricks because they can’t stop their meds or their skin is too irritated.
But here’s the catch: testing too many things at once creates false positives. If you order a panel of 20 allergens, you’re statistically likely to get 5 or 6 positive results-even if you’re not allergic to most of them. That’s why guidelines say: only test what makes sense based on your history. A 2025 national guideline found that 38% of inappropriate tests happen when people are retested for foods they’ve eaten safely for years.
Understanding Your Results: Numbers Don’t Tell the Whole Story
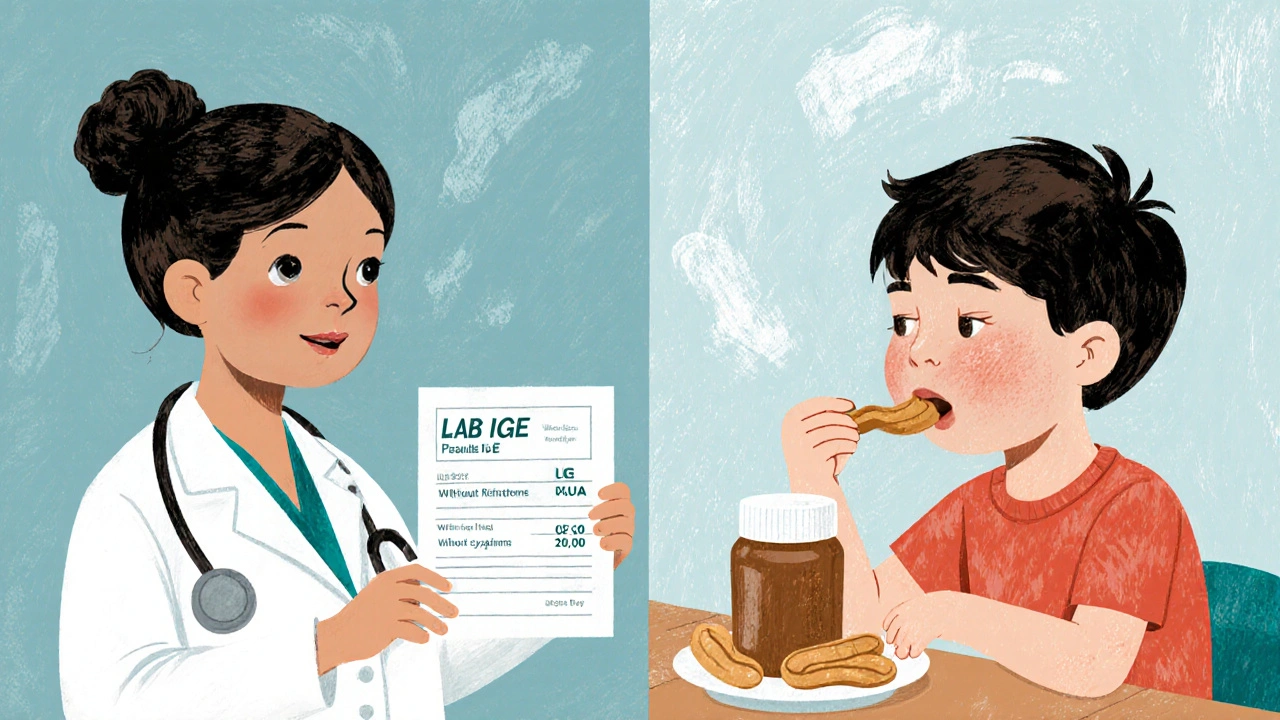
Your report might say 0.5 kUA/L for peanut. That’s above 0.35, so it’s ‘positive.’ But does that mean you’ll go into anaphylaxis if you eat peanut butter? Not necessarily.
Higher numbers mean higher likelihood. At 0.35 kUA/L, the chance of a true peanut allergy is around 50%. At 15 kUA/L, that jumps to 95%. That’s why doctors don’t just look at one number-they look at the trend. If your peanut IgE has gone from 0.4 to 2.1 over two years, that’s more concerning than a stable 0.6.
And don’t forget total IgE. If your total IgE is 100 kUA/L and your peanut IgE is 0.5, that’s only 0.5% of your total antibodies. But if your total IgE is 1.5 kUA/L and your peanut IgE is 0.5, that’s over 30%. That changes how you interpret the result. Labs now automatically check total IgE when a specific IgE comes back positive, because context matters.
How This Test Compares to Skin Prick Testing
Skin prick testing is still the gold standard when it’s possible. A drop of allergen is placed on your skin, then lightly pricked. If you’re allergic, you get a red, itchy bump within 15 minutes. It’s faster, cheaper, and slightly more sensitive-especially for airborne allergens like dust mites or pollen.
But blood tests have advantages. Skin tests can be dangerous if you’ve had a severe reaction before. They can also be unreliable if you’re on antihistamines, steroids, or certain antidepressants. Blood tests aren’t affected by meds. They’re also better for babies with very sensitive skin or people with widespread eczema.
Studies show skin prick testing is about 15-20% more sensitive for common allergens. But modern blood tests have closed that gap. For food allergies like egg or milk, the accuracy is now very close. The real difference isn’t sensitivity-it’s practicality.
What the Test Won’t Tell You
Specific IgE testing doesn’t diagnose non-IgE allergies. If you get stomach cramps hours after eating dairy but no hives or swelling, that’s likely a non-IgE reaction-maybe lactose intolerance or a food protein-induced enterocolitis. Blood tests won’t pick that up.
It also won’t tell you how much of the allergen you can tolerate. Two people might both have a 3.2 kUA/L result for milk, but one can drink a cup of yogurt without issue, while the other breaks out in hives from a lick of ice cream. That’s why the test is just one piece of the puzzle. Your doctor needs to know: What happened? When? What triggered it?
And forget food mix panels. Testing for ‘tree nuts’ as a group? That’s outdated. A positive result could mean you’re allergic to cashew, but not walnut-or vice versa. Component-resolved diagnostics now test for specific proteins like Ara h 2 in peanuts or Cor a 9 in hazelnuts. These can tell you if you’re at risk for a severe reaction or just have cross-reactivity (like pollen-food syndrome). Labs in the UK are starting to use these, but they’re still only available in specialized allergy centers.

When to Avoid This Test
Don’t get tested if you’ve never had a reaction. No symptoms? No need. A 2025 guideline found that 22% of all specific IgE tests ordered in primary care were unnecessary. People get tested because they’re worried, not because they have evidence of allergy.
Don’t test for things you’ve eaten safely for years. Retesting milk, eggs, or wheat in someone who’s eaten them daily since childhood is a waste of time-and money. It can lead to unnecessary fear and avoidance.
And don’t test more than 12 allergens at once unless you have a clear reason. More tests = more false positives. One study showed panels with 20+ allergens had false positive rates near 60%. That’s not science-that’s noise.
What Happens After the Test
Results usually come back in 3 business days. Most labs run these tests daily, but some rare allergens (like certain insect venoms) have to be sent to specialized centers, which can add extra days.
If your results are positive and match your symptoms, your doctor might recommend avoiding the allergen, carrying an epinephrine auto-injector, or starting immunotherapy (allergy shots or tablets). If results are low or unclear, they might suggest an oral food challenge under supervision-a controlled way to see if you really react.
Remember: this test doesn’t cure anything. It just helps you understand what’s triggering your body. Treatment comes from combining those results with your real-life experience.
What’s New in Allergy Testing
Technology is improving fast. New platforms like the ImmunoSolid Phase Allergen Chip (ISAC) can test for 112 different allergen components from just 20 microliters of blood. That’s a game-changer for complex cases-like someone allergic to multiple nuts or with unclear food reactions.
But these tests are not for everyone. They’re expensive, complex to interpret, and not yet recommended for routine use. Only allergy specialists should order them. Most community labs still use ImmunoCAP or similar platforms that test for 15-20 common allergens: pollen, dust mites, cat, dog, peanut, egg, milk, soy, wheat, shrimp, etc.
One big win: modern tests can detect IgE levels as low as 0.1 kUA/L, with less than 5% variation between runs. That’s more accurate than ever before. But accuracy doesn’t mean certainty. Interpretation still requires experience.
While I appreciate the clinical precision of this breakdown, the persistent over-reliance on IgE titers as diagnostic anchors remains dangerously reductive. The medical community continues to conflate sensitization with clinical allergy-a distinction that has led to unnecessary dietary restrictions, anxiety, and iatrogenic harm in pediatric populations. This is not science; it’s statistical overreach dressed in white coats.
The data on false positives in multi-allergen panels is statistically undeniable. A 2023 meta-analysis in the Journal of Allergy and Clinical Immunology demonstrated that ordering >10 allergens without clinical correlation yields a 58% false positive rate. Yet primary care providers still order 20-plex panels as if they’re grocery lists. This isn’t diagnostic diligence-it’s defensive medicine masquerading as thoroughness.
Love this breakdown!! 🙌 Seriously, so many people panic over a 0.5 kUA/L result and cut out whole food groups. I’ve seen moms quit their jobs because their kid had a borderline peanut result but had eaten peanut butter weekly for 3 years. The real hero here? The oral food challenge. It’s not scary-it’s empowering. Let’s stop letting numbers rule our lives 😊
ImmunoCAP-yes, but only when properly calibrated. And yet, laboratories-especially in the U.S.-still use outdated reference ranges. The 0.35 kUA/L cutoff? Arbitrary. Derived from a 1992 cohort. Modern assays can detect 0.1. Why are we still using 30-year-old thresholds? This is not science-it’s institutional inertia. And component-resolved diagnostics? Still underutilized. Pathetic.
One thing missing here is the role of IgE in non-IgE mediated reactions. I’ve had patients with chronic GI symptoms and negative IgE tests who responded dramatically to elimination diets. The overemphasis on IgE blinds us to other immune pathways-like IgG4, mast cell activation, or even gut permeability. This test is useful, but it’s not the whole immune story.
my cousin got tested for like 15 things after a rash and got 6 positives. she stopped eating everything and lost 20 lbs. turns out she was just stressed and had a fungal infection. the test didn’t help-her doctor’s listening did. why do we trust numbers more than people?
Let’s be real-this whole IgE testing industry is controlled by Big Pharma and lab conglomerates. Why do you think they pushed these expensive panels? Because they make billions. Meanwhile, real doctors who use history and physical exams? They’re being pushed out. And don’t get me started on how they’re replacing skin tests with blood draws to avoid liability. It’s not medicine-it’s profit-driven fearmongering. Wake up.
Wait so IgE is just a marker? But what if IgE is not the real issue? What if it's the microbiome? Or epigenetics? Or maybe the allergens are modified by pesticides and GMOs? We're measuring the symptom, not the cause. And why do we assume allergy is a 'disease'? Maybe it's the body's way of saying 'this environment is toxic'? You're all missing the forest for the trees. Also, I think the 0.35 cutoff is wrong because I read it on a blog once.
Biggest takeaway? Don’t test unless you have a clear history. I’ve seen so many parents panic over a positive test for milk in a toddler who drinks it daily. If it ain’t broke, don’t test it. And if you’re gonna test, test smart-don’t throw the kitchen sink at it. Also, component testing is the future, but it’s still niche. Keep it simple, stay grounded, and trust your doc if they’re actually listening to you.