Sirolimus and Wound Healing: Surgical Complications and Timing
Sirolimus Timing Calculator
This tool helps determine the optimal time to start sirolimus after kidney transplant surgery based on your specific risk factors. The goal is to balance rejection prevention with safe wound healing.
Recommendation
Results will appear here after calculation
When a patient gets a kidney transplant, the goal isn’t just to keep the organ alive-it’s to keep them alive and healthy for years to come. That’s where sirolimus comes in. But here’s the catch: while it’s great at preventing rejection and lowering cancer risk, it can also slow down wound healing. And when you’ve just had major surgery, that’s not just a side effect-it’s a real threat.
What Sirolimus Does to Healing
Sirolimus, also known as rapamycin, works by blocking a protein called mTOR. That’s useful in transplants because it stops the immune system from attacking the new organ. But mTOR isn’t just involved in immunity-it’s also critical for healing. When you cut your skin, your body sends out signals to rebuild tissue. Fibroblasts move in to make collagen. Blood vessels grow to bring oxygen and nutrients. Immune cells clean up debris. Sirolimus shuts down all of that. Studies in rats show that at therapeutic doses (2.0 to 5.0 mg/kg/day), sirolimus reduces wound breaking strength by up to 40%. Collagen, the main structural protein in skin and connective tissue, drops significantly. The drug also cuts VEGF-the molecule that tells blood vessels to grow-by more than half. Without enough VEGF, wounds don’t get the blood supply they need to close properly. The result? Slower healing, higher risk of opening up, and more infections.When Do Complications Happen?
The biggest risks come in the first week after surgery. That’s when the body is most active trying to repair tissue. If you start sirolimus too soon, you’re essentially hitting pause on the healing process. Many transplant centers delay starting sirolimus for at least 7 to 14 days after surgery. Some wait even longer, especially if the patient had a large incision, like from a kidney transplant. But it’s not just timing. The type of surgery matters too. A small skin biopsy or mole removal? The risk is low. A major abdominal operation? That’s where things get dangerous. A 2008 Mayo Clinic study looked at 26 transplant patients on sirolimus who had dermatologic surgery. Their wound dehiscence rate was 7.7%-compared to 0% in those not on sirolimus. It wasn’t statistically significant, but the trend was clear. The odds of complications jumped sevenfold. And then there’s the problem of lymphocele-a fluid-filled sac that forms near the transplant site. Sirolimus increases this risk by interfering with lymphatic repair. One study found lymphocele rates nearly doubled in patients started on sirolimus too early.Who’s at Highest Risk?
Not everyone on sirolimus will have problems. But some people are much more vulnerable. Obesity is a big one. A higher BMI means more tension on the wound, less blood flow, and more fat tissue that doesn’t heal well. Studies show the odds of healing issues rise with every point increase in BMI. Diabetes is another. High blood sugar messes with collagen and immune function. Smoking? It cuts oxygen delivery and damages blood vessels. Protein malnutrition? Your body can’t rebuild tissue without enough amino acids. Even age plays a role. Older patients heal slower naturally. Combine that with sirolimus, and the risk multiplies. What’s interesting is that some of these risks are fixable. If you’re planning surgery, quitting smoking at least four weeks before helps. Getting your blood sugar under control. Making sure your protein intake is high. These aren’t just nice-to-haves-they’re part of the treatment plan.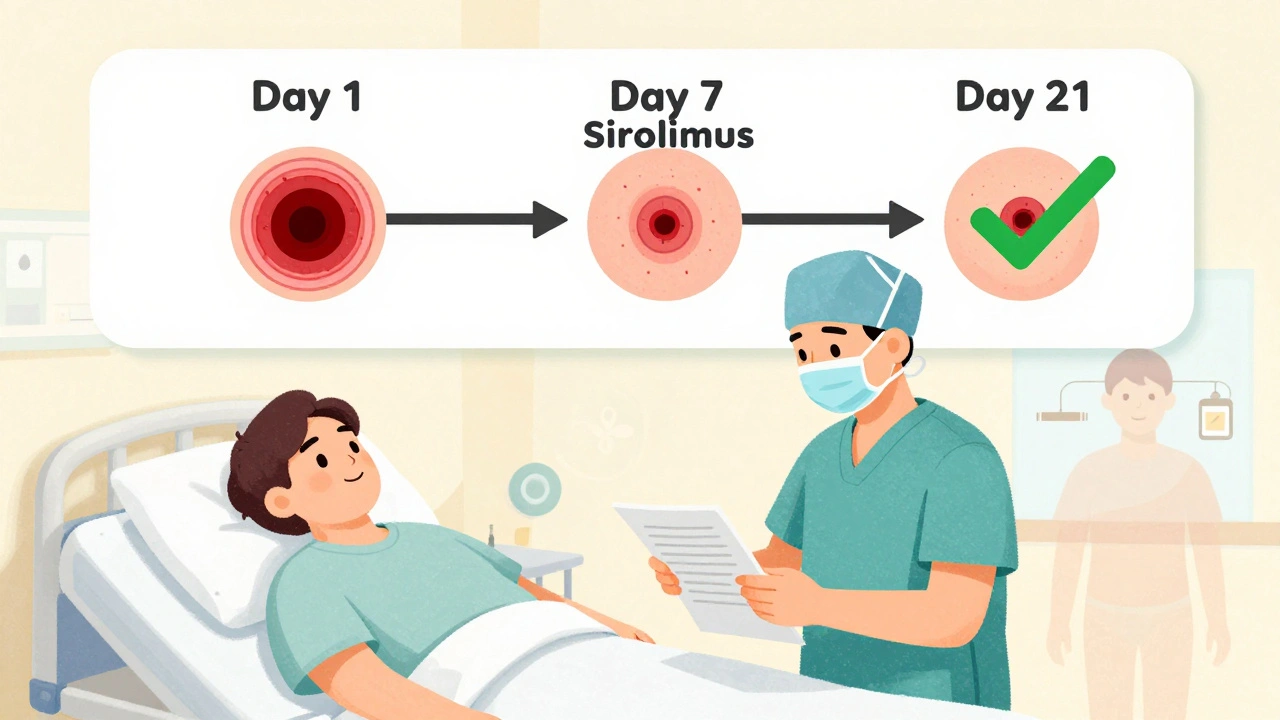
Old Myths vs. New Realities
Ten years ago, most doctors avoided sirolimus entirely after transplant. The warnings were loud: “Don’t start it until healing is complete.” But over time, experience changed that. A 2022 review in Wiley found that many of the early horror stories-wounds bursting open, infections spreading-were from patients who were poorly managed. They started sirolimus too soon. They didn’t optimize nutrition. They didn’t monitor drug levels. Now, centers are learning to use it smarter. Instead of waiting 14 days for everyone, they’re tailoring timing to the patient. Someone with a low BMI, no diabetes, no smoking history? They might start sirolimus at day 7. Someone with obesity, poor nutrition, and a history of slow healing? They wait until day 21 or longer. Trough levels matter too. Keeping sirolimus blood levels between 4 and 6 ng/mL during the first 30 days seems to strike the right balance-enough to prevent rejection, not so much that it kills healing. Higher levels? Higher complication rates.How It Compares to Other Drugs
Sirolimus isn’t the only immunosuppressant that affects healing. Steroids, mycophenolate, and antithymocyte globulin (ATG) all slow down tissue repair. But here’s the difference: steroids weaken collagen and cause skin thinning. Mycophenolate can cause mouth ulcers and GI issues. ATG can trigger cytokine storms. Sirolimus doesn’t cause kidney damage like tacrolimus or cyclosporine. That’s why it’s still used-especially in patients with early signs of kidney toxicity from other drugs. It also lowers skin cancer risk, which is huge for transplant patients who are 65 to 250 times more likely to develop squamous cell carcinoma. So it’s not about avoiding sirolimus. It’s about choosing the right drug for the right patient at the right time.
What Doctors Do Now
Leading transplant centers don’t use a one-size-fits-all rule anymore. They follow a checklist:- Assess wound risk: BMI, diabetes, smoking, nutrition, age
- Delay sirolimus until at least day 7 post-op for high-risk patients
- Start low: 1 mg/day, titrate slowly to target trough of 4-6 ng/mL
- Monitor wound closely for signs of dehiscence or infection
- Hold sirolimus if wound breaks open or infection develops
- Reintroduce only after healing is confirmed
What Patients Should Know
If you’re on sirolimus or about to start it after surgery:- Don’t assume you’re safe just because your doctor says “it’s fine.” Ask: “What’s my risk based on my BMI, diabetes, and smoking history?”
- Stop smoking. At least 4 weeks before surgery. Better yet, quit for good.
- Get your protein intake checked. Aim for 1.2-1.5 grams per kilogram of body weight daily.
- Keep your blood sugar stable. Even prediabetes can delay healing.
- Report any redness, swelling, or fluid leaking from your incision immediately.
- Know that sirolimus isn’t the enemy-it’s the timing and your body’s condition that matter.
The Future of Sirolimus Use
The American Society of Transplantation updated its guidelines in 2021 to reflect this shift. They now say: “Timing of mTOR inhibitor initiation should be individualized based on surgical complexity, patient risk factors, and graft function.” Researchers are now testing wearable sensors that monitor wound oxygen levels and inflammation markers in real time. If a wound is healing well, the system could alert the team to start sirolimus sooner. If not, it delays it. And long-term? Sirolimus is here to stay. For patients with high cancer risk or those who develop kidney damage from other drugs, it’s often the best option. The goal isn’t to avoid it-it’s to use it wisely.Can sirolimus be started right after surgery?
Most transplant centers avoid starting sirolimus in the first 7 days after major surgery due to its interference with tissue repair. For high-risk patients-those with obesity, diabetes, or poor nutrition-waiting 14 to 21 days is common. For low-risk patients with small incisions, initiation at day 7 may be safe with close monitoring and controlled dosing.
Does sirolimus cause more infections after surgery?
Yes, but indirectly. Sirolimus doesn’t directly cause infections like antibiotics do. Instead, by slowing wound closure, it gives bacteria more time to enter and establish infection. Studies show higher rates of wound infections and lymphocele formation when sirolimus is started too early. The risk is highest in patients with poor nutritional status or uncontrolled diabetes.
Is sirolimus safer than tacrolimus for kidney transplants?
It depends. Tacrolimus is more effective at preventing acute rejection but causes kidney damage over time. Sirolimus doesn’t harm the kidneys and reduces cancer risk, making it better for long-term use. However, it carries higher risks for wound healing complications. Many patients switch from tacrolimus to sirolimus after the first year, once the wound has fully healed and rejection risk drops.
Can I take sirolimus if I’m planning another surgery?
If you’re on sirolimus and need elective surgery, your transplant team will likely hold it for at least 7-14 days before and after the procedure. The exact timing depends on your wound risk profile, the type of surgery, and your current drug levels. Never stop sirolimus without medical supervision-this can trigger organ rejection.
Are there alternatives to sirolimus if wound healing is a concern?
Yes. Mycophenolate mofetil is often used as a first-line alternative because it has less impact on wound healing. Steroids are also used, though they come with their own side effects like weight gain and bone loss. For patients at high cancer risk, sirolimus may still be preferred, but only after optimizing healing conditions and delaying initiation.
Bro this is wild - sirolimus is basically a saboteur for your incision. I saw a guy’s graft site split open like a bad zipper after they started it on day 5. No joke, he needed three more surgeries. Don’t be that guy who listens to the nurse and not the science.
There’s something quietly beautiful about how medicine is finally moving away from rigid protocols. It’s not about ‘never’ or ‘always’ - it’s about listening to the body’s quiet whispers before you hit the gas on immunosuppression. 🌱
It is axiomatic that the pharmacological inhibition of the mammalian target of rapamycin constitutes a profound perturbation of the cellular homeostatic equilibrium, particularly with regard to fibroblastic proliferation and angiogenic signaling pathways. Consequently, the temporal initiation of such agents must be contingent upon the empirical validation of wound integrity, lest iatrogenic morbidity ensue.
Wait so you’re telling me my uncle’s wound didn’t close because of this drug? I’ve been blaming his bad diet but what if it’s ALL YOUR FAULT? I’m crying now. Why didn’t anyone tell me? I feel so guilty. I didn’t even know he was on this stuff. Are you sure it’s not just because he’s old? I hate that he’s old. I hate that I didn’t visit more.
One must contemplate the metaphysical paradox of sirolimus: it preserves life by suppressing the very mechanism that restores it. Is healing not the soul’s first act of rebellion against entropy? And yet, we, the architects of modern medicine, choose to throttle it - not out of malice, but out of fear of another kind of death. The tragedy is not in the drug - it is in our hubris to believe we can time the rhythm of tissue with a calendar.
Look i get it sirolimus is a beast but if you’re not smoking and you got a BMI under 25 and your sugar’s good you can start it at day 7 no problem. I’ve seen it work. Just don’t be lazy and skip the protein. Eat eggs. Drink milk. Stop eating junk. Simple.
Let me tell you something - this isn’t just about drugs or timing. This is about dignity. Every patient deserves to heal with their whole body, not just their new kidney. If you’re on sirolimus, you’re not just surviving - you’re choosing to live longer, healthier, with less cancer. But that gift comes with responsibility. Quit smoking. Eat your protein. Check your numbers. This isn’t a suggestion. It’s your new daily ritual. You got this.
Everyone’s acting like sirolimus is some new villain. Newsflash - steroids do way more damage to skin. Tacrolimus nukes your kidneys. Mycophenolate gives you diarrhea 24/7. Sirolimus just slows healing - which you can fix by not being a fat smoker with diabetes. Stop blaming the drug and fix your lifestyle. You think your grandma’s 80-year-old body heals fast? No. So why are you surprised?
So if you’re low risk - day 7 ✅
High risk - day 21 🤝
And protein? Non-negotiable 🥚
Smoking? Quit. Like, yesterday. 🚭
Just… please don’t be the person who makes us all look bad. 💪
Why are we even talking about this like it’s complicated? Just don’t start it until the wound looks like a normal scar. Duh. Also why is everyone so obsessed with protein? I eat pizza and I’m fine. Also I don’t trust any doctor who uses the word ‘trough’ like it’s a magic word. 😴