Shared Decision-Making in Autoimmune Care: How Patients and Doctors Balance Risks and Benefits Together

Why Your Autoimmune Treatment Shouldn’t Be a Guess
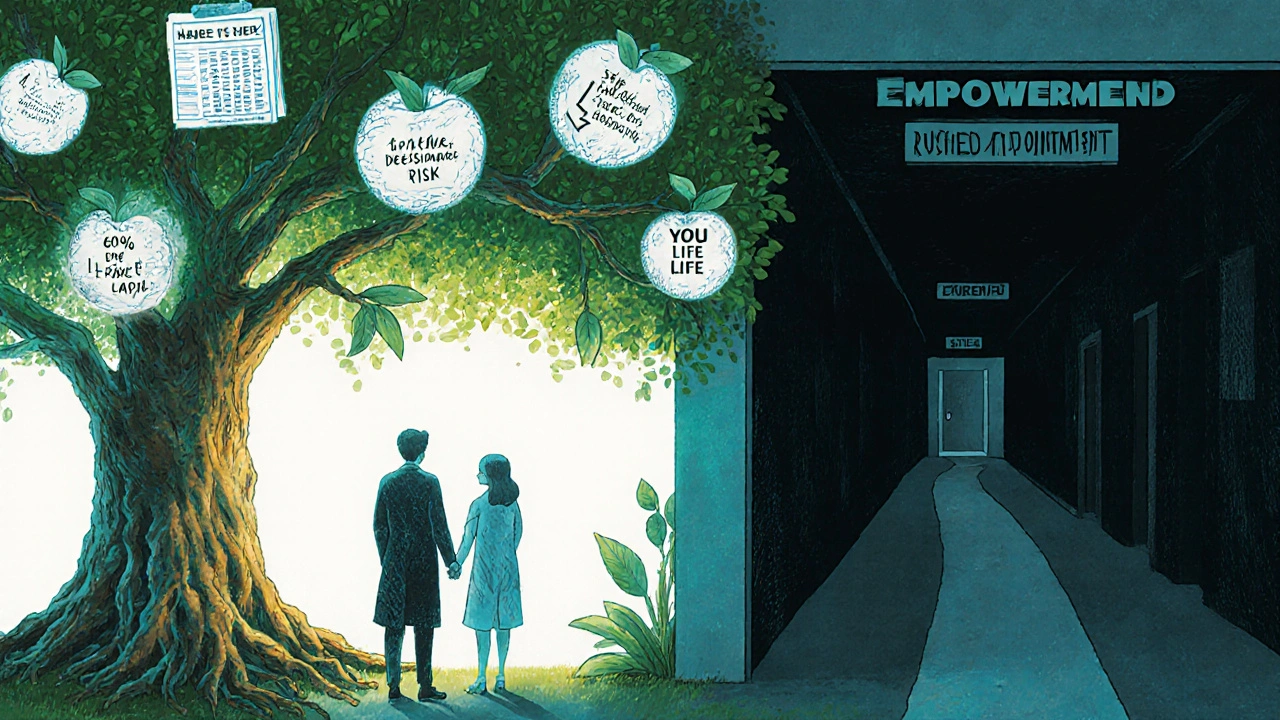
When you’re living with lupus, rheumatoid arthritis, multiple sclerosis, or another autoimmune condition, every treatment choice feels heavy. One drug might slash your flare-ups by 60%, but it could also raise your risk of a rare brain infection by 1 in 1,000. Another might be easier to take-just a pill-but it won’t stop the disease as well. And then there’s your job, your family, your fear of needles, your travel schedule, your budget. No doctor can decide this for you. And no app or website can either.
That’s where shared decision-making comes in. It’s not just a buzzword. It’s the difference between taking a drug because your doctor said so-and taking it because you understand exactly what you’re signing up for.
What Shared Decision-Making Really Looks Like
Shared decision-making isn’t about handing you a brochure and saying, “Pick one.” It’s a structured conversation. Three steps. That’s it.
- Team talk: “I want us to make this decision together. What matters most to you right now?”
- Option talk: “Here are your choices. This drug reduces flares by 60%. But 1.8 out of every 100 people on it get a serious infection each year. This one has a 0.1% chance of PML over two years-that’s 1 in 1,000.”
- Decision talk: “Which option lines up with your life? Let’s pick one, or try something else.”
This takes 9 to 14 minutes. Not 90 seconds. Not a rushed appointment where you nod along while the doctor lists three drug names. Studies show patients who go through this process stick with their treatment 82% of the time. Those who don’t? Only 63%.
Why Numbers Matter-And Why Percentages Can Trick You
Doctors used to say things like, “This drug cuts your risk of relapse by 50%.” Sounds great, right? But if your baseline risk was only 2%, cutting it in half means going from 2% to 1%. That’s not a miracle. That’s a small gain.
Good shared decision-making uses absolute numbers. Not relative. Not vague. Real numbers you can picture.
- “Of 100 people like you, 60 will see big improvement with this biologic.”
- “Of those same 100, 2 will get a serious infection in the next year.”
- “1 person in 1,000 might develop PML after two years on this drug.”
That’s how you know if the trade-off is worth it. A 2017 study found patients who saw absolute risks were 37% less likely to make choices based on fear or misunderstanding.
Tools That Actually Help-Not Just Fancy Apps
You don’t need a high-tech app to make good decisions. But you do need tools that turn numbers into meaning.
The Arthritis Foundation offers free, printable decision aids for RA, lupus, and psoriatic arthritis. They show side effects in simple charts. The National MS Society’s “MS Values” tool asks you to rank what matters: avoiding relapses? Staying off injections? Keeping your job? It then matches your answers to treatment options.
One tool from the University of Michigan, called “MS Decisions,” shows PML risk as “1 in 1,000 over two years,” not “0.1%.” Patients rated it 4.6 out of 5. Why? Because they could finally see what it meant.
And there’s new tech. In March 2023, the FDA cleared the first AI-powered decision tool for rheumatoid arthritis-ArthritisIQ. It pulls data from your EHR, your symptoms, your lifestyle, and builds a personalized risk-benefit profile. But even this tool works best when a doctor walks you through it.
When Shared Decision-Making Doesn’t Work
It’s not magic. It doesn’t fix everything.
When you’re in a severe flare-your joints screaming, your vision blurring, your legs giving out-there’s no time for a 14-minute chat. Doctors often skip SDM then. And that’s okay. Emergency treatment isn’t about choice. It’s about survival.
But here’s the problem: too many doctors skip SDM even when there’s time. A 2021 survey found 78% of rheumatologists say they don’t have enough time. Only 22% consistently use decision aids-even though 89% say they believe in them.
And if you’re over 65, or if English isn’t your first language, or if you’ve struggled with health literacy before, digital tools alone won’t help. You need someone to sit with you, explain slowly, and check if you really understood.
What Patients Are Saying
On patient forums like CreakyJoints and Reddit’s r/rheumatoidarthritis, people keep saying the same thing:
“When my rheumatologist showed me actual numbers, I felt like I could finally breathe. I chose the drug that let me keep traveling for work-even if it meant more injections.”
“I was told to take methotrexate. I didn’t know it could cause liver damage. I didn’t know there were other options. I felt stupid for asking questions. I wish someone had asked me what I wanted.”
One woman with MS, a nurse working night shifts, was pushed toward an injectable therapy. She didn’t say no. She just didn’t say yes either. She stopped taking it. Two years later, she had her third relapse. She told her neurologist: “You never asked me if I could handle needles every other day.”
That’s the cost of skipping shared decision-making. Not just a bad choice. A broken trust.
What’s Changing-and What’s Still Missing
Things are moving. The American College of Rheumatology and the American Academy of Neurology both now recommend shared decision-making as standard care. Medicare ties 9% of payments to patient experience scores-and SDM is a big part of that. The European League Against Rheumatism now requires doctors to document SDM before starting biologics. In Europe, that’s led to 22% more appropriate prescriptions.
But here’s the gap: only 32% of U.S. providers document SDM in records. Insurance doesn’t always pay for it. Training is still rare. Most doctors never learned how to do this in med school.
And patients? They’re still waiting. A 2020 survey by the National MS Society found 63% of patients felt rushed during treatment talks. One wrote: “My neurologist listed three MS drugs in 90 seconds. No discussion. No visuals. Just ‘take one.’”
What You Can Do Today
You don’t need to wait for your doctor to lead. You can start this conversation.
- Before your appointment, write down: What matters most to you? (Work? Family? Avoiding shots? Keeping your energy?)
- Ask: “What are my options? What are the real risks-like how many people actually get this side effect?”
- Ask: “Do you have a tool or handout that shows the numbers?”
- Ask: “If this were your mom or your sibling, what would you recommend?”
Bring a friend. Take notes. Use the free tools from the Arthritis Foundation or the National MS Society. You don’t have to be an expert. You just have to be heard.
The Bottom Line
Autoimmune diseases don’t have one right answer. There’s no single best drug. There’s only the best drug for you.
Shared decision-making isn’t about giving you more choices. It’s about making sure the choice you make fits your life-not just your lab results.
It’s the difference between taking a drug because you were told to-and taking it because you truly believe it’s the right one. And that’s the only kind of treatment that lasts.
Is shared decision-making only for biologics?
No. Shared decision-making applies to every major treatment choice in autoimmune care-whether you’re choosing between methotrexate and sulfasalazine, deciding whether to start an oral drug like tofacitinib, or weighing the pros and cons of switching from an injectable to an infusion therapy. It’s especially important when options have similar effectiveness but different side effects, dosing schedules, or lifestyle impacts.
What if my doctor doesn’t want to do shared decision-making?
It’s not uncommon. Some providers still operate under the old model where they make the call. If your doctor dismisses your questions, try saying, “I’ve read that shared decision-making improves outcomes in autoimmune diseases. Can we use a decision aid together?” If they still resist, consider asking for a referral to a provider trained in patient-centered care. Many rheumatology and neurology clinics now have specialists who focus on this approach.
Do I need to be highly educated to use shared decision-making?
No. Decision aids are designed for all literacy levels. Tools from the Arthritis Foundation and National MS Society use simple language, visuals, and real-life examples. If numbers are confusing, ask your provider to explain them using stories-like “Out of 100 people like you, 60 will feel much better.” The goal isn’t to understand statistics. It’s to understand what matters to you.
Can shared decision-making make my condition worse?
Not if it’s done right. In fact, studies show it reduces decisional conflict and increases treatment adherence, both of which improve long-term outcomes. The risk comes from skipping it-choosing a treatment that doesn’t fit your life, leading to early discontinuation, uncontrolled disease, and more hospital visits. Shared decision-making helps you avoid those pitfalls.
Are there free tools I can use before my appointment?
Yes. The Arthritis Foundation offers free, downloadable decision aids for rheumatoid arthritis, psoriatic arthritis, and lupus. The National MS Society has the “MS Values” tool online. Both are designed for patients, not clinicians. You can use them alone or bring them to your appointment to start the conversation. Many patients say using these tools helped them feel more confident and less anxious during their visits.
This is the kind of post that makes me believe medicine can still be human. I've been on three different biologics for RA and no one ever sat down with me like this. Just 'take this, come back in 3 months.' I wish I'd known about absolute numbers back then. I'd have picked differently.
frankly i dont trust docs who use big words. if u gotta explain 1 in 1000 like its rocket science then u r not doing ur job. i just wanna know if i gonna die or be able to play with my kids. simple.
I'm a nurse and I've seen this play out so many times. Patients who understand the numbers don't just stick with treatment-they feel empowered. One patient I worked with, she had MS and was terrified of injections. We used the MS Values tool and found she valued independence over reducing relapses by 10%. She chose the oral med. She's been stable for 4 years now. This isn't just nice-it's necessary.
The real issue is time. Doctors want to do this but they're scheduled every 12 minutes. If insurance paid for 20-minute consults instead of 8, this would become standard. No magic. Just better reimbursement. Also the tools from Arthritis Foundation are gold. Print them. Bring them. Don't wait for the doctor to offer.
I read this and immediately thought about my mom. She had lupus and her doctor told her 'this drug is 70% effective' and she took it. Turns out 70% of what? 70% of people who don't have kidney damage? 70% of people who aren't 70 years old? She never asked. She just trusted. And now she's on dialysis. This post should be mandatory reading for every patient with an autoimmune disease. Seriously.
Oh, here we go again. The 'shared decision-making' fairy tale. Let me guess-next you'll tell us that patients should also decide which antibiotics to use for sepsis? This isn't 'empowerment,' it's medical theater. You don't need to 'understand' PML risk to know that a 0.1% chance is astronomically low. Most patients are emotionally compromised. They don't want charts. They want a doctor who knows what they're doing. This whole movement is just another way for med-school grads to feel virtuous while billing less.
I used to think this was all fluff until my sister with RA started using the decision aids. She came to her appointment with a printed chart, wrote down her priorities, and asked for the absolute numbers. The rheumatologist actually smiled. Said, 'I wish more patients did this.' She’s been on her drug for a year now. No flares. No regrets. It’s not complicated. Just human.
I'm just here to say this whole 'shared decision-making' thing is just a fancy way of saying 'I don't want to be responsible.' You want to know what's really dangerous? Letting someone who Googles 'lupus symptoms' at 2am choose their treatment. I've seen it. People panic. They refuse meds because they read a blog about 'toxicity.' Then they end up in the ER. Doctors are trained. Patients are scared. Stop pretending we're all equal in this. It's not collaboration. It's chaos dressed in mindfulness.
The ethical imperative of shared decision-making cannot be overstated. Autonomy, beneficence, non-maleficence-these are not abstract principles. They are the bedrock of clinical ethics. When patients are presented with absolute risk figures, their capacity for informed consent is materially enhanced. The documented increase in adherence rates (82% vs. 63%) is not merely statistically significant-it is morally compelling. Institutional adoption must be accelerated, not delayed by administrative inertia.
I used to think this was just corporate buzzword bingo. Then I got diagnosed with MS. I sat in that office, terrified, and the neurologist didn't say 'take this.' He said, 'Tell me what you're afraid of.' I said I didn't want to lose my job. He pulled up the tool. Showed me 1 in 1,000. Said, 'You're more likely to die in a car crash on your way home than get PML.' That moment? Changed everything. Not because of the number. Because he asked me what mattered. That's all anyone needs.
I'm from the UK and we're starting to see this shift here too. NHS is piloting decision aids in several rheumatology clinics. The best part? Patients actually show up for follow-ups. I think it's because they feel like they're part of the team, not just a case number. This isn't just good medicine-it's good for the system. Less wasted appointments. Fewer drug switches. Everyone wins.
So let me get this straight. We're supposed to believe that giving patients a chart with numbers magically fixes a system built on profit, time constraints, and doctor ego? You think the 78% of rheumatologists who say they don't have time are just lazy? Or is it that the system actively disincentivizes this? This post is beautiful. But it's a Band-Aid on a hemorrhage. We need to fix the machine, not teach patients how to beg for dignity.