Red Flag Drug Combinations to Avoid for Safer Treatment

Every year, thousands of people die not from taking one drug, but from mixing them. It’s not always illegal substances-sometimes it’s your prescription painkiller, a nightcap, or that anxiety pill you took earlier. The real danger isn’t just using drugs alone. It’s combining them. Some pairings don’t just add risk-they multiply it. And the consequences aren’t theoretical. They’re deadly.
Why Mixing Drugs Is More Dangerous Than You Think
Most people think if a drug is legal or prescribed, it’s safe. But that’s not true when it’s mixed with another substance. Alcohol, benzodiazepines, opioids, stimulants-they don’t just coexist in your body. They interact. And those interactions can shut down your breathing, stop your heart, or fry your liver. The body doesn’t treat drugs like separate events. It processes them together. When two drugs affect the same system-like your brain’s control over breathing-things go wrong fast. Even a small amount of alcohol with a low dose of an opioid can be enough to cause respiratory arrest. You don’t need to be a heavy user. You just need to mix two things that shouldn’t be mixed.The Deadliest Combo: Opioids + Alcohol
This is the most common lethal combination. Opioids like oxycodone, hydrocodone, and fentanyl slow down your breathing. Alcohol does the same. Together, they don’t just add up-they team up. Research shows this mix increases the risk of respiratory depression by 4.5 times compared to either drug alone. People often don’t realize how little it takes. One glass of wine with a single oxycodone pill after dental surgery has landed people in emergency rooms, requiring naloxone to reverse the overdose. The sedation isn’t just drowsiness. It’s loss of consciousness, coma, or death. And because alcohol masks the intensity of opioid effects, users often take more, thinking they can handle it. They can’t.Benzodiazepines + Opioids: A Silent Killer
Benzodiazepines-Xanax, Valium, Ativan-are prescribed for anxiety and sleep. They’re powerful CNS depressants. When paired with opioids, they create a perfect storm. In 2020, over 30% of opioid-related overdose deaths also involved benzodiazepines. That’s not a coincidence. It’s a pattern. These drugs work on the same brain receptors. Together, they amplify sedation, muscle weakness, and breathing suppression. Even people who take their prescriptions exactly as directed can overdose if they drink alcohol or use another depressant. The CDC found that 78% of fatal opioid overdoses involved at least one other substance-and benzodiazepines were the second most common after alcohol. In 2019, Medicare started requiring pharmacies to flag these combinations in their prescription systems. The result? A drop of 18% in co-prescribing. But the problem persists. Many patients aren’t warned clearly. Others don’t realize their anxiety med is part of the danger.The Speedball: Cocaine + Heroin
This combo is called a “speedball.” It’s a myth that cocaine cancels out heroin’s sedation. It doesn’t. It just makes you feel like you’re in control when you’re not. Cocaine speeds up your heart and raises blood pressure. Heroin slows your breathing and lowers your heart rate. Your body is being pulled in two directions at once. The result? Extreme stress on your cardiovascular system. Heart attacks, aneurysms, and sudden cardiac arrest are common. In 2021, nearly half of all cocaine overdoses in the U.S. involved heroin. Celebrities like River Phoenix and John Belushi died from this combo. But it’s not just famous people. It’s happening in homes, garages, and alleyways across the country. The danger is amplified by fentanyl. Most street heroin today contains fentanyl-and you won’t know. One pill, one snort, one shot-and your body can’t handle the load.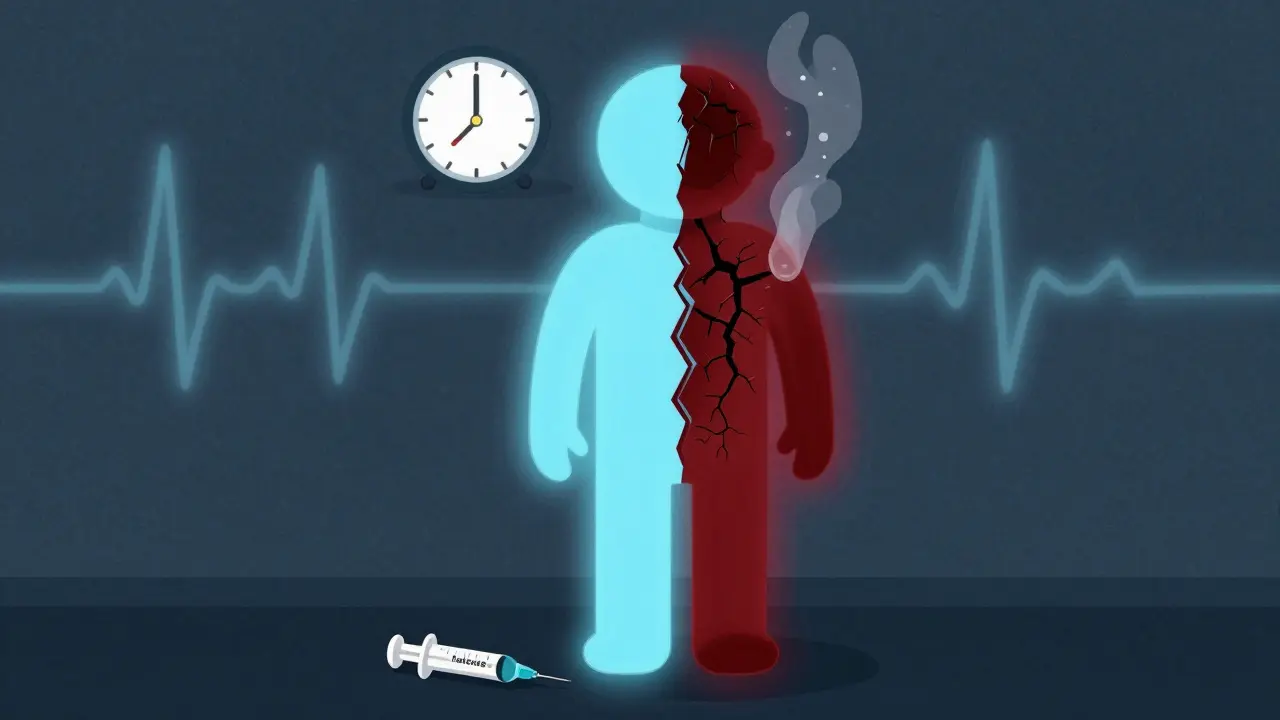
Alcohol + Cocaine: The Hidden Toxin
When alcohol and cocaine are mixed, your liver creates something called cocaethylene. It’s not just a metabolite-it’s a toxin. Cocaethylene lasts longer than cocaine, keeps you high longer, and is 25% more likely to cause sudden death. It also damages your liver. Studies show 65% of chronic users of this combo develop liver toxicity. Symptoms? Severe stomach pain, seizures, irregular heartbeat, coma. And because alcohol dulls your senses, you might not realize how much cocaine you’ve taken. You think you’re fine. Then your heart gives out. This combo is especially dangerous because it feels like it balances out. But it doesn’t. It just makes the crash worse-and the risk of death higher.Antidepressants + Alcohol: A Quiet Hazard
Many people don’t think of antidepressants as dangerous when mixed with alcohol. But they are. Duloxetine (Cymbalta) and venlafaxine (Effexor) can increase liver damage by up to 40% when combined with alcohol. The risk isn’t just long-term. It can happen after one night of drinking. Alcohol lowers your tolerance for these drugs. It can trigger sudden dizziness, fainting, or even suicidal thoughts. In one study, alcohol lowered the threshold for fatal overdose with venlafaxine by 25%. That means someone who could normally handle a certain dose of the drug might die from half that amount if they’ve had even one drink. And it’s not just these two. SSRIs and SNRIs can also increase bleeding risk when taken with NSAIDs like ibuprofen-especially if you drink. It’s not just about mental health. It’s about physical survival.Buprenorphine + Alcohol: A Trap for Recovery
Buprenorphine is used to treat opioid addiction. It’s lifesaving. But it’s not safe with alcohol. Mixing them can cause severe hypotension (blood pressure below 90/60), dangerously slow breathing (under 10 breaths per minute), and deep sedation that leads to coma. People in recovery often think they’re “safe” because they’re on medication. But alcohol doesn’t care. It still depresses the CNS. And buprenorphine still binds to opioid receptors. Together, they can undo years of progress in minutes. The SA Health Department puts it bluntly: “The more alcohol in the body, the less heroin needed to cause an overdose.” The same applies to buprenorphine. Even a small amount of alcohol can tip the scale.
What You Can Do to Stay Safe
You don’t need to be an addict to be at risk. You just need to be taking more than one substance. Here’s what works:- Read labels. Every prescription bottle now has warnings about alcohol and other drugs. Don’t ignore them.
- Ask your pharmacist. They’re trained to catch dangerous combinations. Don’t assume your doctor told you everything.
- Use a drug interaction checker. Tools like WebMD’s or Medscape’s are free and easy. Type in your meds and alcohol-and see what pops up.
- Be honest with your doctor. If you drink, use cannabis, or take supplements, say so. They can’t help if they don’t know.
- Carry naloxone. If you or someone you know takes opioids-even if prescribed-have naloxone on hand. It can save a life in under two minutes.
The Bigger Picture
The rise in polysubstance overdoses isn’t random. It’s fueled by fentanyl contamination, lack of education, and the false belief that “I know my limits.” But limits don’t matter when drugs interact unpredictably. AI-powered screening tools are now being rolled out in hospitals and pharmacies to flag risky combinations before they’re dispensed. By 2025, these systems will be standard. But technology can’t replace awareness. Your body doesn’t know the difference between a pill from a pharmacy and a powder from a street dealer. It only knows what’s in your bloodstream. And if it’s a dangerous mix, your body won’t survive.Frequently Asked Questions
Can I have one drink if I’m on a prescription opioid?
No. Even one standard drink can double your risk of respiratory depression when combined with opioids. The interaction isn’t linear-it’s exponential. What feels like a small amount can be enough to stop your breathing. The safest choice is no alcohol at all.
Are over-the-counter painkillers safe with alcohol?
Not always. Acetaminophen (Tylenol) combined with alcohol can cause severe liver damage-even at normal doses. NSAIDs like ibuprofen can increase stomach bleeding risk when mixed with alcohol, especially if taken regularly. Always check the label or ask a pharmacist before combining.
I’m on antidepressants. Is it okay to have a beer on weekends?
It depends on the medication. Some, like venlafaxine or duloxetine, significantly increase liver toxicity with alcohol. Others may worsen drowsiness or depression. Even if you feel fine, the risk is still there. Talk to your prescriber before drinking. There’s no universal green light.
Why do people mix drugs if it’s so dangerous?
Many believe they can control the effects-like using cocaine to counteract opioid sedation. Others don’t know the risks. Some are self-medicating for anxiety, pain, or trauma. And with fentanyl in so many street drugs, users often don’t even know what they’re taking. Education and harm reduction are key.
What should I do if someone overdoses from a drug combo?
Call 911 immediately. If you have naloxone, administer it right away-even if opioids aren’t confirmed. Naloxone is safe and can reverse opioid-related respiratory failure. Stay with the person until help arrives. Don’t leave them alone. Time is critical.
My cousin OD’d on oxycodone and wine after his back surgery. They found him blue in the bathroom. He was 22. No one told him one glass was enough. I still see his face every time I drink.
Just saw a study from Johns Hopkins last week: 72% of ER visits from polysubstance interactions involved people who thought they were ‘just having one drink’ with their meds. The body doesn’t do ‘just one.’ It does ‘total system failure.’ Always check interactions. Even if it’s ‘just’ ibuprofen and beer.
Doctors prescribe these combos all the time and act surprised when people die. They’re not trying to kill you but they don’t care enough to learn. The system is broken. Naloxone should be in every pharmacy like aspirin.
Wow. I read this while sipping my chamomile tea and suddenly felt guilty about that one time I had wine with my antidepressant. Maybe I should’ve asked my pharmacist instead of Googling ‘does this kill you’ at 2am.
Of course it’s dangerous. People are stupid. You don’t mix chemicals unless you’re a chemist. And even then you’d wear gloves. But no, let’s just throw everything in one pot and call it ‘self-care.’
This hit hard. My mom’s on buprenorphine and drinks one glass of wine every night to sleep. She says it’s ‘just one.’ I’m printing this out and putting it on her fridge. She needs to see it in black and white.
They say fentanyl is in everything but they’re lying. This whole thing is a government scam to push naloxone and control the poor. People have been mixing alcohol and painkillers since the 1800s and nobody died. Until now. Coincidence?
They’re hiding the truth. The FDA knows about cocaethylene. They’ve known since 1998. But Big Pharma doesn’t want you to know because then no one would buy Xanax or Adderall anymore. It’s all about profit. Wake up.
Man, this is the kind of post that makes you pause mid-sip. I used to think ‘I’ve got this’ with my meds and a beer. Now I just drink tea and feel weirdly proud of it. Small wins, right?
The grammatical inaccuracies in the original post are egregious. The misuse of ‘they’re’ in place of ‘their,’ the inconsistent capitalization of ‘CDC,’ and the improper use of em dashes in place of hyphens undermine the credibility of what is otherwise a scientifically sound argument. One cannot trust the message if the messenger cannot master basic orthography.