Polysomnography: What to Expect During a Sleep Study and How Results Are Interpreted
Have you ever felt exhausted even after a full night’s sleep? Or heard from your partner that you stop breathing while asleep? If so, you might be dealing with a sleep disorder-and polysomnography could be the key to understanding why.
What Is Polysomnography?
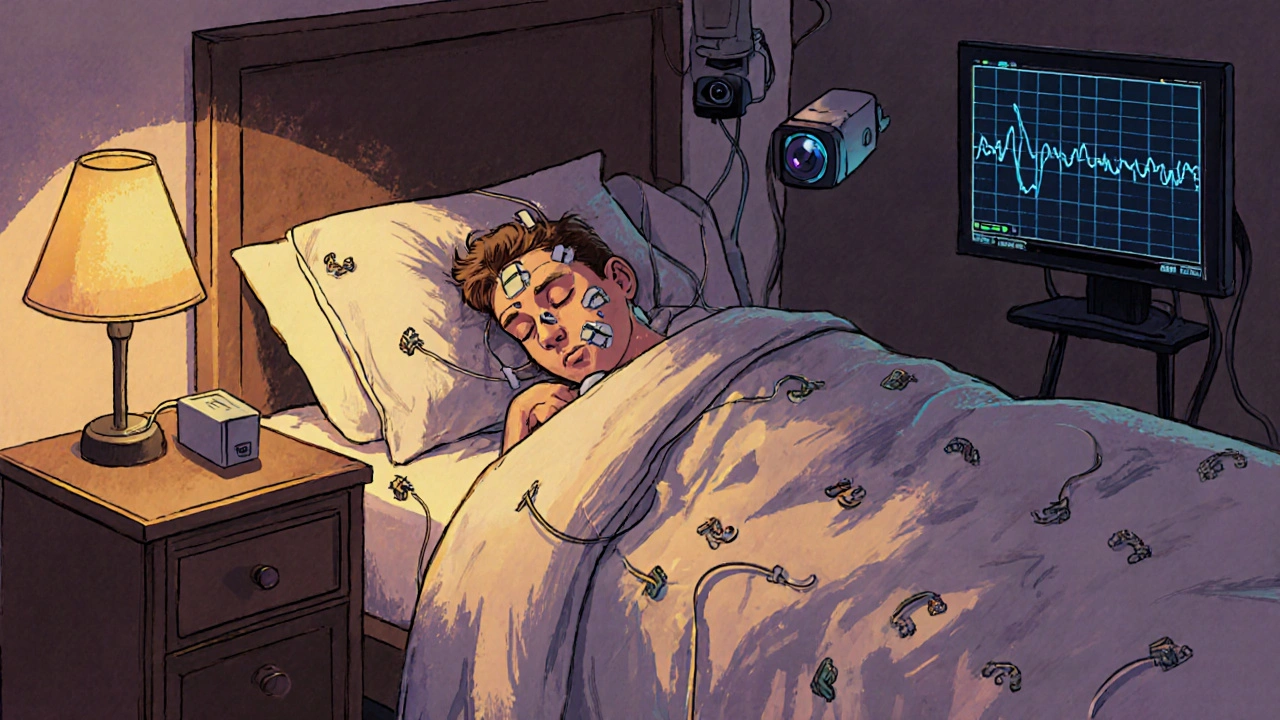
Polysomnography, often called a sleep study, is the most detailed way doctors diagnose sleep disorders. It’s not just about counting how many times you wake up. It’s about watching your brain, eyes, heart, breathing, and muscles all night long to see how your body behaves during sleep. The word itself breaks down simply: poly means many, somno means sleep, and graphy means recording. So, polysomnography is a multi-parameter sleep recording. And it’s the gold standard-not because it’s fancy, but because it works. Unlike a home sleep test that only tracks breathing and oxygen levels, polysomnography records at least seven key signals: brain waves, eye movements, muscle activity, heart rhythm, breathing effort, airflow, and blood oxygen. It even records your body position and snoring with video. This full picture lets doctors tell the difference between sleep apnea, narcolepsy, restless legs, night terrors, and other conditions that all cause daytime fatigue-but need totally different treatments.What Happens During a Sleep Study?
You’ll arrive at a sleep center about an hour before your usual bedtime. The room looks like a hotel room: comfortable bed, quiet, temperature kept between 68-72°F. No hospital feel. But you’ll notice the wires. A sleep technologist will attach about 22 small sensors to your scalp, face, chest, legs, and fingers. These aren’t needles. They’re sticky patches and soft bands. You’ll feel them, but you won’t feel pain. The wires connect to a small box beside your bed. You can still move, roll over, even use the bathroom-the tech can pause the recording if you need to get up. You’ll be asked to avoid caffeine after noon the day before. Don’t nap. Stick to your normal sleep schedule. The goal is to capture your real sleep, not an artificial version. Once you’re settled, the lights go out. The technologist watches you from another room through a camera and microphone. They can talk to you if you’re uncomfortable. Most people fall asleep within an hour. Even if you don’t sleep as well as you do at home, it’s usually enough for diagnosis. About 85% of people complete the study successfully. The whole thing lasts 6-8 hours-enough time to cycle through all sleep stages: light sleep, deep sleep, and REM sleep. That’s important because disorders like narcolepsy mess with the order of these stages. In a healthy person, REM sleep doesn’t come until after 90 minutes. In someone with narcolepsy, it can hit right away.What Does the Data Show?
After the study, a board-certified sleep doctor spends 2-3 hours reviewing the data. That’s over 1,000 pages of raw numbers and waveforms. Here’s what they’re looking for:- Apnea-hypopnea index (AHI): How many times per hour your breathing stops or gets shallow. AHI of 5-15 is mild sleep apnea. 15-30 is moderate. Over 30 is severe.
- Sleep architecture: How much time you spent in each sleep stage. If you’re not getting enough deep sleep or REM sleep, it explains why you’re tired.
- Oxygen drops: If your blood oxygen falls below 90% for more than 10 seconds, that’s a red flag. Frequent drops mean your body isn’t getting enough air.
- Leg movements: Periodic limb movements during sleep can fragment your rest, even if you don’t wake up.
- Abnormal behaviors: Sleepwalking, screaming, or punching the air? Video helps confirm parasomnias like REM sleep behavior disorder.
- Heart rhythm changes: Irregular beats during sleep can signal underlying heart issues tied to sleep apnea.

Polysomnography vs. Home Sleep Tests
You might have heard about home sleep tests. They’re cheaper, and you sleep in your own bed. So why not just do one? Home tests usually track only 3-4 things: airflow, oxygen, breathing effort, and heart rate. They’re good for spotting moderate to severe sleep apnea-but they miss almost everything else. Here’s the difference:| Feature | In-Lab Polysomnography | Home Sleep Test |
|---|---|---|
| Parameters Monitored | 7-16 (brain waves, eye movements, muscle tone, heart, breathing, oxygen, position, video) | 3-4 (airflow, oxygen, breathing effort, heart rate) |
| Can Diagnose Narcolepsy? | Yes | No |
| Can Diagnose Restless Legs? | Yes | No |
| Can Diagnose Parasomnias? | Yes | No |
| Failure Rate | 2-5% | 15-20% |
| Cost | Higher (often covered by insurance) | 30-50% cheaper |
Split-Night Studies: Diagnosis and Treatment in One Night
Sometimes, the sleep doctor sees clear signs of severe sleep apnea early in the night. Instead of making you come back, they might switch to a split-night study. After the first 2-3 hours of diagnostic recording, they’ll wake you up gently and fit you with a CPAP mask. Then they’ll adjust the air pressure while you sleep to find the level that keeps your airway open. By morning, you’ll have both a diagnosis and a treatment plan. About 35% of polysomnography studies today are split-night. It saves time, reduces stress, and gets people on therapy faster.What Do the Results Mean for You?
Your doctor will get a full report within 7-10 days. It won’t just say “you have sleep apnea.” It’ll break down:- How bad it is
- What type (obstructive, central, or mixed)
- Whether you need CPAP, oral appliance, surgery, or behavioral changes
- If you also have another disorder like periodic limb movement disorder
Common Concerns and Myths
“I won’t be able to sleep with all those wires.”Most people do sleep enough. The sensors are lightweight. The room is quiet. And the tech is there to help you relax. If you only get 4 hours of real sleep, that’s often enough. “Is this covered by insurance?”
Yes, if it’s medically necessary. Medicare covers 80% of the cost. Most private insurers require a referral from your doctor and documented symptoms like loud snoring, witnessed apneas, or excessive daytime sleepiness. “Can’t I just use a Fitbit or Apple Watch?”
No. Wearables track movement and heart rate. They can guess if you were asleep. But they can’t measure brain waves, breathing effort, or oxygen drops. They’re not medical devices. “What if I’m a light sleeper?”
That’s normal. The lab environment is unfamiliar. But you don’t need a perfect night. You need enough data to see patterns. One night of fragmented sleep can still show clear signs of a disorder.
What Comes After the Study?
Once you have your results, your doctor will explain them in plain terms. You’ll get a treatment plan. For sleep apnea, that often means a CPAP machine. You’ll get fitted for a mask, trained on how to use it, and scheduled for a follow-up in 3-6 months. If the study shows something else-like REM behavior disorder or narcolepsy-you’ll be referred to a neurologist or sleep specialist who handles those conditions. The goal isn’t to make you dependent on machines. It’s to help you wake up feeling rested. To stop your partner from sleeping in the guest room. To reduce your risk of stroke, high blood pressure, and heart disease.Final Thoughts
Polysomnography isn’t glamorous. It’s not a quick fix. But for people struggling with unexplained fatigue, loud snoring, or sudden sleep attacks, it’s often the only way to get real answers. It’s not about being judged for how you sleep. It’s about being helped to sleep better. If you’ve been told you’re “just tired,” or if your sleep has been off for months or years-don’t accept that. Ask your doctor about a sleep study. The answer might change your life.Is polysomnography painful?
No, polysomnography is not painful. Sensors are attached with adhesive patches and soft belts-no needles or invasive procedures. You may feel slight discomfort from the wires or mask, but most patients report no significant pain. The biggest challenge is adjusting to sleeping in a new environment, not the equipment itself.
How long does it take to get results from a sleep study?
Results typically take 7 to 10 business days. After your study, a sleep technologist reviews the raw data, then a board-certified sleep physician interprets the findings. This process involves analyzing over 1,000 pages of information, including brain waves, breathing patterns, oxygen levels, and sleep stages. Your doctor will schedule a follow-up to discuss the report and next steps.
Can I use my phone or watch TV before bed during the study?
You can use your phone or read before lights out, but screen time should be limited. Bright screens can delay sleep onset by suppressing melatonin. Most sleep centers allow you to bring personal items like books or tablets (in airplane mode) to help you relax. Once the study begins, you’ll be asked to turn off electronics to avoid interference with the sensors.
Do I need to stay overnight for a polysomnography?
Yes, standard polysomnography requires an overnight stay in a sleep center. The test needs to capture a full sleep cycle, including multiple transitions between NREM and REM sleep, which only occurs during natural, uninterrupted sleep. While home sleep tests exist, they don’t provide the same level of detail and cannot diagnose disorders like narcolepsy or parasomnias.
What if I have to use the bathroom during the study?
You can get up anytime. The sensors are connected to a portable box, and the technologist can quickly disconnect the wires so you can walk to the bathroom. You’ll be given a gown with easy access, and the setup is designed to allow mobility. Most people use the bathroom once or twice during the night without issue.
Are there alternatives to in-lab polysomnography?
Yes, home sleep apnea tests (HSAT) are available for patients with high suspicion of moderate to severe obstructive sleep apnea and no other sleep disorders. These tests monitor airflow, oxygen, and breathing effort-but not brain waves, eye movements, or leg movements. They’re cheaper and more convenient, but they can’t diagnose narcolepsy, REM behavior disorder, or periodic limb movement disorder. If your symptoms are complex, your doctor will likely recommend an in-lab study.
Does insurance cover polysomnography?
Most insurance plans, including Medicare, cover polysomnography when ordered for a diagnosed medical need. Common qualifying symptoms include loud snoring, witnessed breathing pauses, excessive daytime sleepiness, or a history of hypertension and obesity. Prior authorization is often required. Always check with your provider, but coverage is standard for medically indicated studies.
Polysomnography isn’t just a test. It’s a doorway to better health. For many, it’s the first step out of years of exhaustion, frustration, and unanswered questions. If you’re tired of living in a fog, it might be time to ask for help.
Been through this twice - first time I thought I’d never sleep again with all those wires, but honestly? The tech was so chill she had me laughing before lights out. Woke up feeling like I’d actually slept for the first time in years. If you’re tired of being a zombie, just do it. No regrets.
They say polysomnography is the gold standard - but isn’t that just another way of saying ‘we monetize your exhaustion’? We’ve turned sleep, the most primal human experience, into a data farm where your dreams are barcoded and sold to Big Pharma. You think they care if you get rest? They care if you buy a CPAP machine next quarter.
And don’t get me started on split-night studies. It’s not medicine, it’s a corporate efficiency hack. You’re not getting help - you’re getting streamlined.
Meanwhile, the real issue? Our culture glorifies burnout. We’re all just sleep-deprived zombies trying to out-sleep each other in a hamster wheel of productivity. The machine doesn’t fix that. It just gives you a new gadget to feel guilty about.
And yet… I still did it. Because even a broken compass points north sometimes.
Oh wow, another ‘sleep study’ that makes you feel like a lab rat in a 1950s sci-fi flick. I’m just here waiting for the moment someone says ‘your REM cycles are statistically abnormal’ and then quietly slips you a pill labeled ‘Regulate Your Existential Dread’.
Also, why is everyone acting like this is revolutionary? My cat sleeps better than I do - and she doesn’t have 22 electrodes glued to her face.
Just had my study last month and the AHI was 38 - severe apnea. CPAP changed my life. No more 3pm crashes, no more ‘did I just fall asleep in the shower’ moments. The mask is weird at first but you get used to it. And yes the room is weird but you sleep more than you think. Don’t overthink it just go
Everyone’s so obsessed with the machine but no one talks about the emotional toll. You’re lying there in this sterile room, wired up like a science experiment, wondering if your brain is broken. And then the tech says ‘you had 47 apneas last hour’ - and suddenly your whole identity becomes ‘sleep-disordered person’.
They give you a diagnosis like it’s a trophy. But what about the shame? The fear that your partner will leave you because you snore like a chainsaw? The guilt that you’re not ‘just tired’ - you’re medically defective?
This isn’t medicine. It’s a mirror that reflects your deepest insecurities back at you in graph form.
Why do people still think this is necessary? I’ve seen 50 people with sleep apnea. All of them were overweight, drank alcohol, and slept on their backs. Fix the lifestyle. No machine needed.
Let’s be real - this whole system is designed to keep you dependent. CPAP machines cost $1,200. Insurance ‘covers’ them but only after you jump through 17 hoops. Meanwhile, the sleep centers make bank on every split-night study. It’s not healthcare. It’s a subscription service for tired people.
And don’t even get me started on the ‘you need this because you’re a danger to yourself’ guilt-trip. I’m not a pilot. I’m not a trucker. I just want to wake up without feeling like I ran a marathon in my sleep.
But hey - if you want to spend $2,000 to prove you’re broken… go ahead. I’ll be over here, sleeping on the couch… quietly.
OMG I DID THE STUDY AND IT WASNT EVEN BAD?? Like I thought I’d be like ‘oh no the wires are gonna suffocate me’ but nooo the tech was so sweet she gave me a weighted blanket and played lofi beats through the speaker. I slept 5.5 hours which is like a record for me. And my AHI was 42 but now I have a CPAP and I feel like a new person. Like I actually remember what sunlight feels like. YALL NEED TO DO THIS. NO EXCUSES.
Have you ever wondered why polysomnography is only available in ‘sleep centers’ and never in your own home? Why the government doesn’t fund home-based neuro-monitoring systems? Why the data is locked behind proprietary software owned by three corporations? This isn’t medicine - it’s a surveillance protocol disguised as care. They’re not measuring your sleep. They’re measuring your compliance.
And if you think your insurance covers it? Think again. They’ll deny you based on ‘insufficient documentation’ - then charge you $800 for the ‘follow-up consultation’ you never asked for.
The real diagnosis? Capitalism has turned rest into a commodity.
I was terrified to do this - I’m a light sleeper and hate being watched. But the staff made it feel so human. They asked if I wanted the lights dimmed earlier, if I preferred the fan on, if I wanted to bring my own pillow. That little kindness meant more than the machine ever could.
I had mild apnea. The CPAP helped, but what changed me most was realizing I wasn’t ‘just tired.’ I had a real issue. And that made me feel seen, not judged.
If you’re hesitating - go. You deserve to wake up feeling like yourself.
In India, we say ‘jagran’ - the night vigil. But here, sleep is a performance. We are expected to sleep like machines - eight hours, uninterrupted, perfectly staged. Polysomnography is the ultimate audit of that performance. We are not allowed to be tired. We are not allowed to be human.
I did the study. My AHI was 18. But what they didn’t measure? The grief I carried. The anxiety that kept me awake. The fact that I was still thinking about my mother’s funeral when the machine recorded my REM cycles.
Maybe the real disorder isn’t in my breathing… but in how we’ve forgotten how to rest.
It is imperative to underscore the clinical indispensability of polysomnography as the unequivocal diagnostic modality for the comprehensive evaluation of sleep architecture and associated pathophysiological phenomena. The reductionist reliance upon home-based sleep apnea tests constitutes a significant epistemological and therapeutic deficit, particularly in the context of complex, comorbid, or neurologically mediated sleep disorders. To equate the two modalities is to conflate a rudimentary screening tool with a definitive diagnostic instrument of unparalleled granularity. One must, therefore, exercise rigorous discernment when considering alternative pathways to care.