Polycystic Ovary Syndrome: Understanding Hormonal Imbalance and Fertility Treatment
What Is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome, or PCOS, isn’t just about cysts on the ovaries. It’s a hormonal disorder that affects 5 to 10% of women during their reproductive years. The name comes from the appearance of the ovaries on ultrasound-packed with small, immature follicles that look like cysts. But the real problem isn’t the cysts. It’s the hormonal chaos behind them.
Three things define PCOS: irregular or absent periods, signs of too many male hormones (like facial hair or acne), and polycystic ovaries on scan. You only need two of these three to get diagnosed. Many women don’t realize they have it until they try to get pregnant. On average, it takes 2 to 3 years after symptoms start to get a correct diagnosis. That’s a long time to feel confused, frustrated, or even blamed for something that’s not your fault.
How Hormones Go Wrong in PCOS
The core issue in PCOS is a broken feedback loop between the brain, ovaries, and metabolism. It starts with insulin resistance. About 50 to 70% of women with PCOS-even those who aren’t overweight-have cells that don’t respond well to insulin. The body responds by pumping out more insulin. That extra insulin doesn’t just affect blood sugar. It tells the ovaries to make more testosterone.
Normal testosterone levels for women are around 15 to 25 ng/dL. In PCOS, they often hit 30 to 50 ng/dL. That’s why 70% of women with PCOS develop hirsutism (excess hair on the face, chest, or back), 30 to 40% get severe acne, and 25% notice thinning hair on the scalp. At the same time, high insulin lowers SHBG, a protein that binds testosterone. That means more free testosterone is circulating and causing trouble.
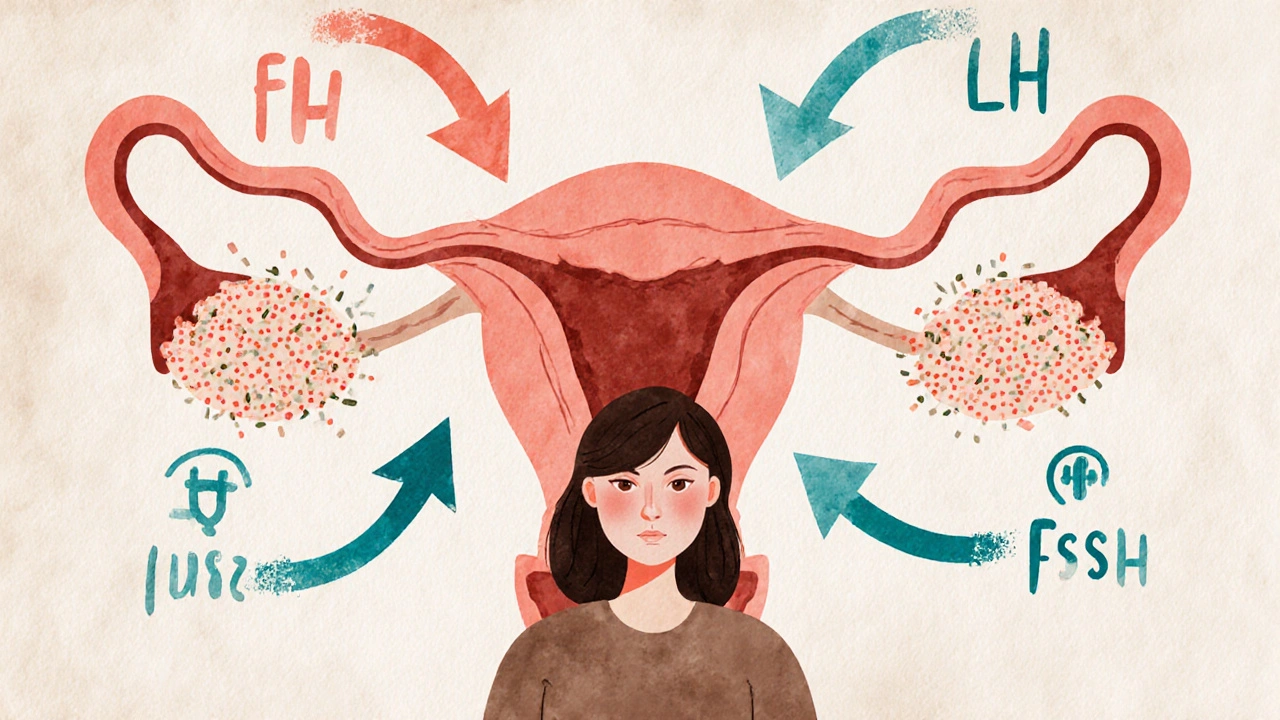
Then there’s the brain. The pituitary gland releases too much luteinizing hormone (LH) and not enough follicle-stimulating hormone (FSH). Normally, FSH helps follicles mature so one can release an egg. In PCOS, LH is too high, FSH is too low, and follicles get stuck. No egg released = no period. No period = no progesterone. That leaves estrogen acting alone, which can thicken the uterine lining and raise the risk of endometrial cancer over time.
Fertility Treatment: Where to Start
If you’re trying to get pregnant and have PCOS, your first step isn’t medication. It’s lifestyle. Losing just 5 to 10% of your body weight can restore ovulation in up to half of women with PCOS. That doesn’t mean extreme dieting. It means steady changes: walking 30 minutes most days, eating more vegetables and whole grains, cutting back on sugary drinks and processed snacks.
Studies show that following the Diabetes Prevention Program plan-150 minutes of moderate exercise per week and cutting 500 to 750 calories daily-helps 60% of women lose enough weight to start ovulating again. And for many, that’s all they need.

Medications That Help You Ovulate
If lifestyle changes aren’t enough, doctors turn to medication. Clomiphene citrate (Clomid) has been the go-to for decades. It works by tricking the brain into releasing more FSH. About 60 to 85% of women on Clomid will ovulate, and 30 to 40% will get pregnant within six cycles. But it doesn’t work for everyone. About 1 in 5 women don’t respond.
For those who don’t respond to Clomid, letrozole (Femara) is now the preferred choice. A major 2014 study found that women taking letrozole had higher ovulation rates (88% vs. 70%) and better live birth rates (27.5% vs. 19.1%) than those on Clomid. Letrozole works by lowering estrogen slightly, which signals the brain to produce more FSH. It’s not FDA-approved for this use in the U.S., but it’s widely used and recommended by experts because it’s more effective and has fewer side effects.
Metformin, a diabetes drug, is often added to the mix. It helps insulin work better, which lowers testosterone and can restart ovulation. Alone, it’s not as strong as Clomid or letrozole-only 15 to 40% of women ovulate on metformin alone. But when combined with Clomid, pregnancy rates jump by 30 to 50%, especially in women with a BMI over 35 or clear signs of insulin resistance.
When Medications Don’t Work: Advanced Options
If oral meds fail, the next step is injectable fertility drugs called gonadotropins. These directly stimulate the ovaries to produce multiple eggs. They work well-about 15 to 20% of women get pregnant per cycle. But they come with risks. There’s a 20 to 30% chance of twins or triplets, and a 5 to 10% risk of ovarian hyperstimulation syndrome (OHSS), a dangerous condition where the ovaries swell and fluid leaks into the abdomen.
IVF is usually saved for women who’ve tried other options or have other infertility issues like blocked tubes or male factor problems. Women with PCOS respond strongly to IVF drugs, but they need lower doses to avoid OHSS. Still, the risk is higher than in women without PCOS-10 to 20% versus 1 to 5%. That’s why experienced fertility clinics now use gentler protocols and monitor closely with blood tests and ultrasounds.
The Bigger Picture: PCOS Is More Than Fertility
PCOS doesn’t go away after you have a baby. It’s a lifelong condition with serious long-term risks. By age 40, half of women with PCOS will develop type 2 diabetes. Their risk of heart disease is doubled. They’re more likely to have high blood pressure, high cholesterol, and fatty liver disease.
That’s why treatment shouldn’t stop at getting pregnant. Annual blood tests for glucose and lipids are essential. Even if you’re not trying to conceive, managing insulin resistance matters. A low-glycemic diet (foods that don’t spike blood sugar) can reduce insulin levels by 30%. The DASH diet, designed for high blood pressure, has been shown to improve menstrual regularity in 35% of women with PCOS over 12 weeks.
Stress also makes PCOS worse. High cortisol from chronic stress disrupts the same hormonal pathways as insulin resistance. Sleep, mindfulness, and therapy aren’t luxuries-they’re part of treatment.

What No One Tells You About Treatment
Metformin can cause nausea and diarrhea in more than half of users. Many stop taking it within six months because they weren’t told how to start slowly. The trick? Begin with 500 mg once a day with dinner, and increase by 500 mg every week. Most side effects fade by the second month.
Weight stigma is still common in clinics. One survey found 78% of women with PCOS felt judged for their weight during medical visits. That’s not just hurtful-it makes people avoid care. You deserve a provider who treats you with respect and focuses on health, not just numbers on a scale.
And mental health? Depression and anxiety affect 30 to 50% of women with PCOS. Yet only 32% of clinics screen for it. If you’re feeling down, anxious, or hopeless, talk to your doctor. Therapy and sometimes medication can make a huge difference.
What’s New in PCOS Care
Technology is starting to help. In 2022, the FDA approved Femaloop PCOS, an app that gives personalized diet, exercise, and sleep plans based on your symptoms. In trials, it improved menstrual regularity by 28% in six months.
Researchers are also using AI to predict PCOS before symptoms get bad. Algorithms that combine AMH levels, LH:FSH ratios, and ovarian volume can now diagnose PCOS with 92% accuracy. This could lead to earlier intervention-before fertility problems arise.
And new drugs are coming. Relugolix, a pill that blocks LH and balances hormones, showed 89% of women had regular periods in early trials, compared to just 32% on placebo. It’s not available yet, but it’s a sign that better treatments are on the horizon.
You’re Not Alone
PCOS is common. You’re not broken. You’re not failing. You’re dealing with a complex condition that science is still learning to treat well. The good news? We know what works. Lifestyle changes, the right meds, and consistent care can get you to ovulation, pregnancy, and long-term health-even if it takes time.
Start with one step: get your insulin and hormone levels checked. Talk to a doctor who listens. Eat one more vegetable a day. Walk for 20 minutes. These aren’t just steps to fertility-they’re steps to feeling like yourself again.
Can you get pregnant with PCOS?
Yes, most women with PCOS can get pregnant with the right treatment. Lifestyle changes, medications like letrozole or clomiphene, and sometimes IVF can help restore ovulation. Many women conceive within a year of starting treatment, especially with early intervention and support.
Does PCOS go away after pregnancy?
No, PCOS is a lifelong condition. Pregnancy doesn’t cure it. Hormonal imbalances and insulin resistance remain. However, some women notice temporary improvement in symptoms during pregnancy due to hormonal shifts. After delivery, symptoms usually return, so ongoing management is still important.
Is metformin safe for fertility?
Yes, metformin is commonly used to improve fertility in women with PCOS, especially those with insulin resistance. It’s not a first-line fertility drug like letrozole, but when combined with ovulation-inducing medications, it can increase pregnancy rates by 30 to 50%. Side effects like nausea are common but often improve with gradual dosing.
Why do some women with PCOS have normal weight?
PCOS isn’t caused by being overweight. While many women with PCOS are overweight, up to 50% have a normal BMI. The root cause is insulin resistance and genetic factors that affect hormone production. Thin women with PCOS still have high androgens and irregular ovulation-they just don’t carry extra weight as a visible sign.
Can diet alone treat PCOS?
Diet alone won’t cure PCOS, but it’s one of the most powerful tools. A low-glycemic, high-fiber diet can lower insulin levels by 30%, improve ovulation, and reduce androgen symptoms. When combined with exercise and medical care, diet can restore regular periods and even lead to pregnancy without medication in some cases.
What’s the best test to diagnose PCOS?
There’s no single test. Diagnosis requires at least two of three criteria: irregular periods, signs of high androgens (like hair growth or elevated testosterone), and polycystic ovaries on ultrasound. Blood tests for testosterone, LH, FSH, insulin, and thyroid function help rule out other causes. Ultrasound isn’t used for diagnosis in teens because follicles are naturally common in young ovaries.
Can PCOS cause miscarriage?
Yes, women with PCOS have a slightly higher risk of early miscarriage-about 30 to 40% compared to 10 to 15% in the general population. This is linked to insulin resistance, high androgens, and inflammation. Managing insulin with metformin or lifestyle changes before conception can reduce this risk.
Are there natural supplements that help PCOS?
Some supplements show promise, but they’re not replacements for medical treatment. Inositol (especially myo-inositol) has been shown to improve insulin sensitivity and ovulation in multiple studies. Vitamin D deficiency is common in PCOS, and correcting it may help regulate cycles. Omega-3s can reduce inflammation. Always talk to your doctor before starting any supplement, as they can interact with medications.
Just wanted to say this post saved my life. I had no idea my acne and missed periods were linked. Started walking daily and cut soda - guess what? My cycle came back. No meds needed. Thanks for the real talk.
So many women feel alone with this. You’re not broken. You’re not lazy. Your body’s just wired differently. Keep going - small steps add up. You’ve got this.
As someone from India, I’ve seen so many girls told to ‘just lose weight’ - but my cousin? Normal BMI, severe PCOS. She was misdiagnosed for 4 years. This post nails it: insulin resistance isn’t about weight. It’s biology.
Bro, metformin gave me crazy stomach cramps at first 😩 Started at 500mg once a day with dinner - now I’m fine. Trust the process. You’re not alone! 💪
i read this and cried a little. my dr never mentioned insulin or inositol. just said ‘try clomid’ and sent me on my way. thank you for explaining why it’s not my fault.
While the clinical information presented is largely accurate and well-sourced, one must consider the epistemological limitations of reductionist endocrinology in addressing a systemic, multifactorial disorder such as PCOS. The emphasis on pharmacological intervention and metabolic metrics risks reifying biomedical hegemony, potentially obscuring the psychosocial and ecological determinants of hormonal dysregulation. A truly holistic framework must integrate epigenetic, circadian, and sociocultural variables - not merely insulin sensitivity and ovulation rates.
lol so let me get this straight - the same doctors who told me I was ‘too fat’ to get pregnant are now telling me to take a diabetes drug to get pregnant? And letrozole - which is technically for breast cancer - is now the gold standard? And we’re not supposed to question that? 🤔
Also, ‘Femaloop app’? Really? Next they’ll sell us a PCOS smartwatch that vibrates when your cortisol spikes. I’m starting to think this whole thing is a pharmaceutical marketing scheme wrapped in wellness fluff.
OMG YES. They told me to ‘just eat clean’ like that’s gonna fix my testosterone levels?? I’m not a Pinterest board. I’m a human being with a broken feedback loop and zero support. And now they want me to pay for an app? LOL. I’m not buying it. This is all just corporate gaslighting with a side of kale.
Who funded this? Big Pharma? The CDC? The WHO? Letrozole isn’t FDA-approved for PCOS - but it’s pushed anyway. Metformin? A generic drug that costs pennies - yet they’ll sell you a $200 ‘PCOS wellness plan’ on Instagram. The real diagnosis? Profit. The real cure? Stop trusting institutions that profit from your confusion.
Start small. One veggie. One walk. One deep breath. That’s enough. Progress > perfection. You’re doing better than you think.
Just wanted to add - if you’re on metformin and it’s wrecking your stomach, try the extended-release version. Huge difference. Also, magnesium glycinate helps with insulin sensitivity and sleep. Not a miracle, but it helped me. And yes, therapy matters - your brain is part of your endocrine system too.
Why do Western doctors always blame insulin? In my country we treat PCOS with herbs and fasting. You people are too dependent on pills. This is a spiritual imbalance. Your diet is poisoned with sugar and technology. You need to return to nature not to metformin.
They’re lying to you. The real reason you can’t get pregnant is because they’re secretly testing hormones on women to control population growth. I know someone who worked at a clinic - they’re injecting something into the IVF meds. Don’t trust the system. You’re being watched.
Thank you. Seriously. I’ve been told I’m ‘too emotional’ for having PCOS. I’m not. I’m just tired. Of being blamed. Of being told to ‘try harder.’ Of being talked over. I’m not broken. I’m just trying to survive. And this? This is the first time I’ve felt seen.