Pharmacy Sourcing Requirements: Legitimate Drug Procurement Standards to Avoid Counterfeit Medications
Every pill, injection, or capsule that ends up in your hands should come from a trusted source. But in today’s global pharmaceutical market, that’s not always guaranteed. Counterfeit drugs are a real and growing threat - from fake antibiotics to altered cancer medications. The stakes? Patient safety, lives, and trust in the healthcare system. Legitimate drug procurement isn’t just paperwork. It’s the line between healing and harm.
Why Legitimate Sourcing Matters More Than Ever
The World Health Organization estimates that 1% of the global drug supply is counterfeit. That might sound small, but it adds up to $200 billion in fake or substandard medications every year. In the U.S., the problem isn’t just about imported fakes. It’s also about stolen drugs, diverted shipments, and suppliers cutting corners. A hospital in Ohio once had to quarantine $87,000 worth of medication because a distributor’s system failed to provide the required electronic transaction history. That’s not a glitch - it’s a red flag. Legitimate sourcing means knowing exactly where your drugs came from, who handled them, and whether they’ve been stored correctly. It’s not optional. It’s the law.The DSCSA: The Backbone of U.S. Drug Traceability
The Drug Supply Chain Security Act (DSCSA), passed in 2013 and fully enforced by November 27, 2023, changed everything. It requires every entity in the drug supply chain - manufacturers, wholesalers, pharmacies - to exchange electronic, interoperable data on every prescription drug package. That means three things for every shipment:- Transaction Information: What drug, how much, who sent it, who received it
- Transaction History: The full chain of ownership from manufacturer to pharmacy
- Transaction Statement: A legal affirmation that the transaction is compliant
What Makes a Supplier Legitimate?
Not all distributors are created equal. The American Society of Health-System Pharmacists (ASHP) lays out seven non-negotiable criteria for vetting suppliers:- Current FDA registration and state pharmacy licenses
- Proof of compliance with current Good Manufacturing Practices (cGMP)
- Documented quality management systems
- No history of recalls or adverse events tied to their products
- Security measures to prevent theft or diversion
- Financial stability - no fly-by-night operators
- Full DSCSA compliance

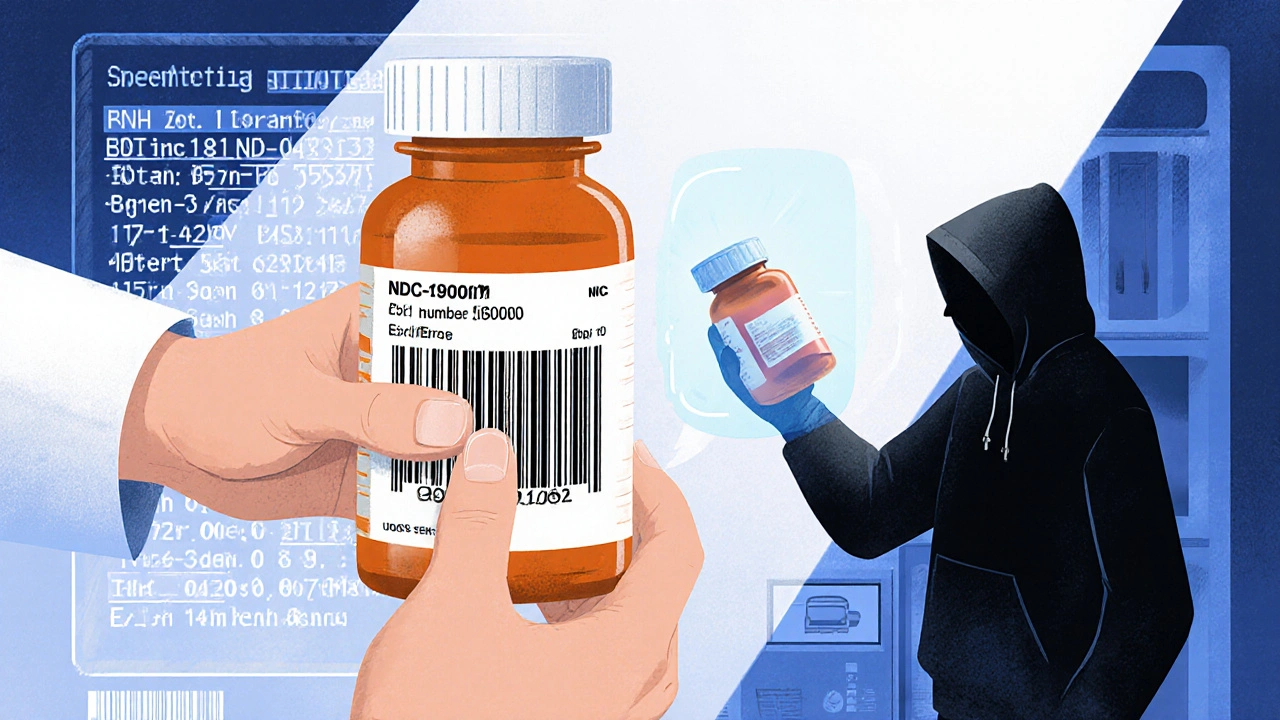
Verification Isn’t Optional - It’s Daily Work
You can’t just take a supplier’s word for it. Legitimate procurement means active, ongoing verification. That includes:- Scanning barcodes on every incoming package to match NDC codes, lot numbers, and expiration dates
- Checking temperature logs for refrigerated drugs (2-8°C for most biologics)
- Keeping transaction records for at least six years
- Conducting quarterly audits of supplier documentation
White Bagging, Brown Bagging, and the Hidden Risks
Some pharmacies try to cut costs by using “white bagging” or “brown bagging” - where patients bring drugs from retail pharmacies to clinics or hospitals. Sounds convenient, right? It’s not. ASHP found that 42% of health systems using these methods had at least one medication error linked to improper handling or lack of verification. A patient might get a drug from a store that didn’t track its temperature during transport. Or the drug might be expired, or even fake. When the clinic administers it, they’re on the hook. No one checks the chain of custody. That’s a legal and clinical disaster waiting to happen.The Real Cost of Cutting Corners
It’s easy to think compliance is just a burden. But the real cost is what happens when it fails. - A patient gets counterfeit cancer drugs that don’t work - they die sooner. - A hospital faces a lawsuit because a batch of insulin was stored at room temperature for days - the patient goes into diabetic shock. - A pharmacy loses its license because they accepted drugs from an unlicensed distributor - they lose their business. The Kaufman Hall Healthcare Finance Report found that compliance costs have jumped 220% since DSCSA started. But the cost of a single counterfeit drug incident? Often millions in fines, lawsuits, and lost trust.
Who’s Winning at Legitimate Sourcing?
Hospitals using Group Purchasing Organizations (GPOs) with dedicated compliance teams had 89% fewer supply chain incidents in 2022. Why? Because GPOs handle the heavy lifting - verifying suppliers, managing DSCSA data, auditing records. They do it at scale, with expertise most small pharmacies can’t afford. Meanwhile, the big distributors - McKesson, AmerisourceBergen, Cardinal Health - control 85% of the U.S. market. They’ve invested millions in blockchain and AI-driven traceability tools. By 2025, 73% of health systems plan to use blockchain to verify drug authenticity. That’s not sci-fi - it’s the new baseline.What’s Changing in 2025 and Beyond
The FDA just got $150 million more in 2024 to fight counterfeit drugs. That means more inspections, more audits, and more penalties. By 2026, AI will analyze supply chain data in real time to flag anomalies - like a sudden spike in orders from an unknown supplier, or a drug moving through a high-risk region. ASHP’s updated guidelines, expected in early 2024, will add stricter rules for compounders and specialty drug suppliers. And states? Thirty-one have added their own rules on top of federal law. One pharmacy in Florida got shut down last year because they didn’t know their state required extra documentation for controlled substances.How to Get It Right
If you’re running a pharmacy, here’s your checklist:- Only buy from suppliers who can prove FDA registration, state licenses, and DSCSA compliance
- Scan every package on arrival - no exceptions
- Keep temperature logs for refrigerated drugs
- Store transaction data for six years
- Train your staff - 120 hours of compliance training isn’t optional
- Use a GPO if you can - it’s cheaper than fines
- Don’t use brown or white bagging unless you have a verified, documented safety protocol
What happens if a pharmacy can’t prove DSCSA compliance?
The FDA can issue warning letters, seize inventory, suspend licenses, or initiate civil penalties. In severe cases, criminal charges can be filed. Pharmacies that repeatedly fail compliance checks are often barred from working with major distributors or government programs like 340B.
Can I buy drugs from international suppliers?
Importing drugs from outside the U.S. is illegal unless it’s for personal use in very limited quantities and meets FDA exceptions. Most international suppliers don’t comply with DSCSA, and their products aren’t subject to U.S. manufacturing standards. Even if the price is lower, the risk of counterfeit or degraded medication is extremely high.
How do I know if a supplier is truly compliant?
Ask for: 1) FDA registration number, 2) State pharmacy license, 3) DSCSA transaction documentation for the last three shipments, 4) Proof of cGMP certification, and 5) A signed compliance attestation. Cross-check the FDA registration at the FDA’s website. If they can’t provide all five, walk away.
Are generic drugs more likely to be counterfeit?
Not inherently. But generics are often targeted because they’re cheaper and less scrutinized. Counterfeiters know people buy them in bulk. The key isn’t brand vs. generic - it’s sourcing. Always verify the supplier, regardless of drug type.
Do small pharmacies have to follow the same rules as hospitals?
Yes. DSCSA applies to all dispensers - hospitals, independent pharmacies, clinics, even mail-order services. The only difference is scale. Small pharmacies may have fewer resources, but the legal requirements are identical. Many use GPOs or third-party compliance services to meet the same standards.
What’s the most common mistake pharmacies make?
Assuming a supplier is legitimate because they’ve been used for years. Suppliers change ownership, get fined, or lose licenses. Compliance isn’t static - it requires continuous verification. One pharmacy in Pennsylvania kept ordering from a supplier for 12 years, then found out the company had been shut down by the FDA in 2021 - they’d been getting drugs from a shell company.
This is the kind of post that makes me want to hug a pharmacist. Seriously, y'all are doing the heavy lifting so we don't end up with fake insulin or expired chemo. 🙏 I work in a small clinic and we just upgraded our scanner last month. Cost us a fortune, but last week it caught a batch of metformin with a mismatched NDC. Called the FDA. Supplier's license got yanked. Worth every penny.
DSCSA is just another gov scam to make small pharmacies go out of business lol who even checks this stuff anyway i mean its just pills right
So let me get this straight - we’re spending 10% of our budget just to verify that a pill wasn’t made in someone’s garage in Shanghai? And we’re supposed to be grateful? 😅 I get it, safety matters. But also… can we just have a national pharmacy monopoly run by the feds and be done with it? Less paperwork, same results. Or at least let me buy my insulin from Canada without getting audited.
Bro this is life or death stuff and people are still acting like it’s a tax audit. Imagine your grandma gets a fake blood pressure pill because someone didn’t scan a barcode. That’s not a ‘mistake’ - that’s a crime. We’re talking about people’s lives here. The tech exists. The laws exist. The will? Not so much. Stop treating compliance like a chore and start treating it like your moral compass. And yeah, GPOs? Total game-changer. They’re the unsung heroes of healthcare. Give them a medal. Or at least a raise.
You think this is about safety? Nah. This is all about control. The big distributors - McKesson, Cardinal - they own the blockchain tech, they own the data, they own the FDA’s ear. Meanwhile, small pharmacies get crushed under paperwork while the same people who run the supply chain are the ones getting rich off it. And don’t even get me started on the 340B program. It’s all a front. The real goal? Monopolize the market and make sure no one else can compete. You think that fake metformin was an accident? Or was it a test? 🤔
Thank you for sharing this important information. It is vital that all pharmacies follow these standards to protect patient health. I hope this message reaches every small practice and clinic. Safety is not optional. It is a responsibility we all share.
The DSCSA is not merely a regulatory framework - it is a necessary and meticulously crafted legal architecture designed to preserve the integrity of the pharmaceutical supply chain. To dismiss it as bureaucratic overhead is not merely ignorant; it is criminally negligent. The fact that anyone would equate compliance with ‘cost’ rather than ‘ethical obligation’ reveals a profound moral failure in contemporary healthcare administration.
I’ve been in this game for 22 years and I’ve seen it all - from the 2012 fungal meningitis outbreak to the time a supplier sent us vials labeled ‘Morphine’ that were actually just sugar water with food coloring. And now they want us to scan every single box? And keep logs for SIX YEARS? And train staff for 120 hours? What about our mental health? What about the fact that my assistant cried last week because she was scared she’d miss a lot number and get sued? This isn’t compliance - this is psychological warfare disguised as patient safety. And don’t even get me started on how the FDA doesn’t inspect the big guys but raids little pharmacies like they’re drug lords. I’m not saying we shouldn’t do it - I’m saying the system is rigged and it’s breaking people.
we started using a gpo last year and it saved us. scanner caught a bad batch too. no more brown bagging. ever. just scan everything. even if its slow.
This makes so much sense. I’m glad someone is finally talking about this clearly.
The implementation of DSCSA-compliant interoperable data exchange protocols necessitates a robust, audit-ready infrastructure for transactional traceability, including NDC validation, lot-level serialization, and real-time cryptographic attestation. Non-compliance constitutes a material breach of 21 CFR Part 203 and exposes entities to liability under the Federal Food, Drug, and Cosmetic Act.
The notion that a small independent pharmacy can meaningfully comply with DSCSA without enterprise-grade ERP integration is not merely optimistic - it is delusional. The regulatory burden has been intentionally structured to consolidate the market. This is not about safety; it is about market consolidation under the guise of public health.
I read this whole thing and I’m just… bored. Like, who cares? If someone gets a fake pill, they’ll know soon enough. And if they die? Well, that’s why we have lawyers. This post reads like a corporate training video written by a robot that hates people.