Patient Assistance Programs from Drug Companies: Eligibility Criteria Explained

Getting life-saving medication shouldn’t mean choosing between rent and refills. But for millions of Americans, that’s the reality. Drug companies offer patient assistance programs (PAPs) to help people afford prescriptions - but the rules aren’t simple. If you’re uninsured, underinsured, or struggling with high out-of-pocket costs, you might qualify. But you need to know exactly who qualifies, what documents they want, and how to avoid common mistakes.
Who Can Get Help?
The biggest myth about these programs is that they’re only for the completely uninsured. That’s not true - but it’s also not the whole story. Most manufacturer PAPs require you to be uninsured or government underinsured. That means if you have private insurance, you’re usually out of luck. But there are exceptions. For example, Pfizer’s Patient Assistance Program won’t help someone whose insurance company tells them to apply for PAP instead. But Merck will consider applicants with insurance if they can prove serious financial hardship. The key? Your insurance can’t be pushing you toward the program. If your plan says, “Apply to the drugmaker for help,” you’re likely ineligible. Medicare beneficiaries face a special challenge. Programs like Takeda’s Help At Hand require you to first apply for Medicare’s Extra Help program. If you’re denied - and your income is below 150% of the Federal Poverty Level - then you might qualify for Takeda’s aid. But if you’re caught in the gap between 135% and 150% FPL? You might not qualify for either. That’s a real hole in the system.Income Limits Are the Main Gatekeeper
Almost every PAP uses income as the deciding factor. And they all use the Federal Poverty Level (FPL) as their baseline. In 2023, 500% of FPL was $75,000 for a single person and $153,000 for a family of four. But here’s where it gets messy: not all programs use the same percentage. Pfizer’s RxPathways uses tiered thresholds. For common drugs like Eucrisa, you must earn less than 300% FPL - about $43,200 for one person. But for expensive cancer drugs, they raise the bar to 500-600% FPL. That’s $64,800 to $77,760 for a single person. GSK sets a fixed cap: $58,650 for one person, $120,570 for four. AbbVie doesn’t set a blanket number - eligibility depends on the specific drug you’re taking. You’ll need to prove your income. Most programs ask for your last tax return, recent pay stubs, or a W-2. Some accept a signed statement if you’re unemployed. But if you use Modified Adjusted Gross Income (MAGI) instead of gross income - a common mistake - your application gets rejected. You must calculate income correctly, including all household members.Insurance Status Can Block You - Even If You’re Broke
This is the hardest part for many people. Independent charity PAPs - like the PAN Foundation or HealthWell Foundation - are more flexible than drugmaker programs. But even they often exclude the uninsured. A 2019 study found 97% of these charities won’t help someone without insurance. That’s ironic, because the uninsured are often the ones who need help most. Manufacturer PAPs are stricter. If you have private insurance, you’re almost always disqualified - unless your plan has a high deductible and you’re spending more than $1,000 a month on meds. Some companies, like AbbVie and Merck, have started “commercial PAPs” for insured patients. These are newer, less known, and usually only cover specific high-cost drugs. You won’t find them unless you dig into the drug’s official website. Medicare Part D beneficiaries have to jump through extra hoops. PAP assistance doesn’t count toward your True Out-of-Pocket (TrOOP) costs. That means if you’re using a PAP to cover your $5,000 insulin, that $5,000 doesn’t help you reach the $8,000 TrOOP threshold needed for catastrophic coverage in 2024. So you’re getting free meds - but still stuck paying more later.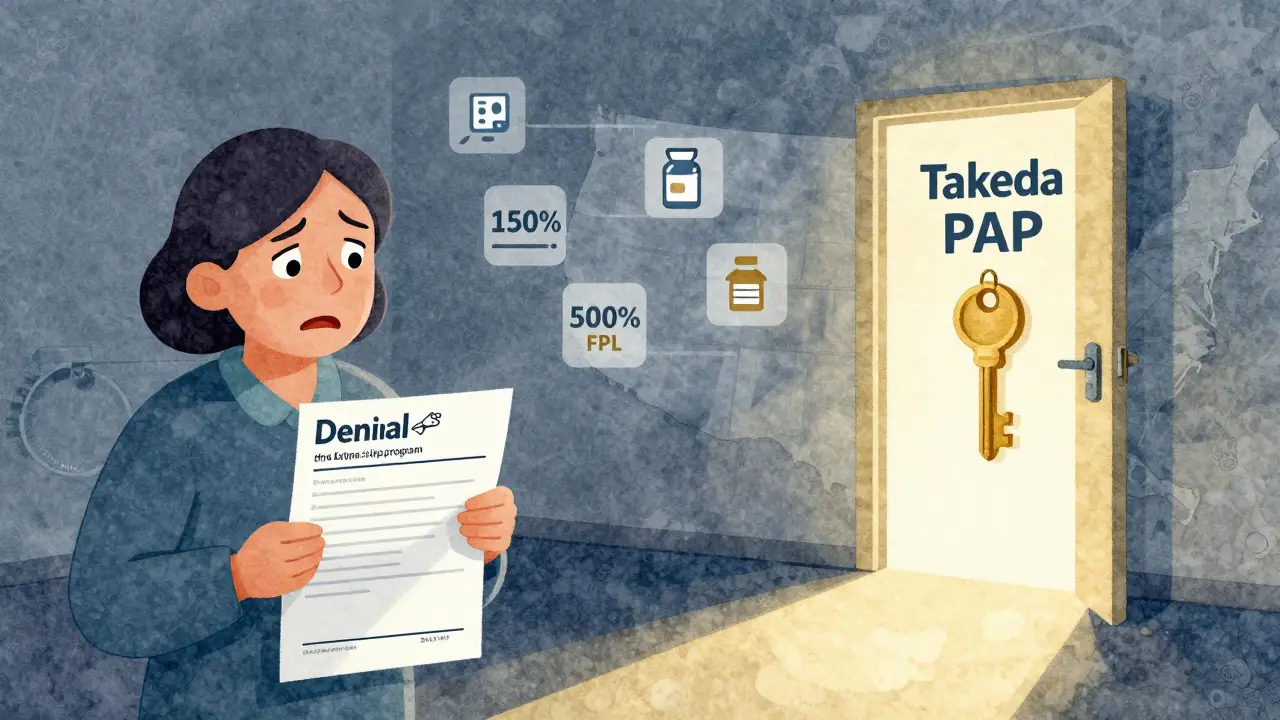
Geographic and Medical Requirements
All programs require you to live in the United States and be treated by a U.S.-licensed doctor. No exceptions. You need to prove your address - a utility bill, lease agreement, or government ID will do. Your doctor must sign off on your application. They’ll need to confirm your diagnosis, that the drug is medically necessary, and that you’re under their care. The drug you’re taking matters too. PAPs focus on brand-name medications, especially high-cost ones. Cancer drugs, rare disease treatments, and biologics are covered at rates above 95%. But generics? Almost never. A 2023 IQVIA analysis showed oncology drugs have 98% coverage through PAPs, while cardiovascular drugs are only 76% covered. If you’re on a cheaper drug, your chances drop.How to Apply - And Why Most People Get Denied
The average application takes 27 minutes. But 68% of denials happen because of incomplete paperwork. You need:- A completed enrollment form (signed by you and your doctor)
- Proof of income (tax return, pay stubs, or affidavit)
- Proof of U.S. residency
- Prescription from a U.S. doctor
- For Medicare users: Denial letter from Extra Help program

What Happens After You Apply?
If approved, you usually get your medication within 72 hours. Some programs ship directly to your home. Others send vouchers to your pharmacy. You’ll need to reapply every 6 to 12 months. GSK requires annual re-enrollment. Pfizer checks income every quarter for specialty drugs. Support is available. About 78% of programs have a dedicated navigator. But wait times are long - 11 minutes on average, 18 minutes for Medicare applicants. Call during business hours. Have all documents ready. Don’t wait until your prescription runs out.What’s Changing in 2025 and Beyond?
The Inflation Reduction Act caps Medicare Part D out-of-pocket costs at $2,000 per year starting in 2025. That will reduce PAP use among seniors by 35-40%. But it won’t fix the problem for the uninsured or underinsured. In fact, with drug prices still rising, PAPs will likely stay critical. Drug companies are slowly making things easier. Pfizer now integrates with TurboTax to auto-fill income data. The Medicine Assistance Tool (MAT) lets you check eligibility across multiple programs at once. But these are still new. Most patients still apply manually.Where to Start
First, identify your drug. Go to the manufacturer’s website. Look for “Patient Assistance,” “Support,” or “Help.” Don’t trust third-party sites - they’re often outdated. Use the Medicine Assistance Tool (MAT) from NeedyMeds. It’s free, accurate, and covers 90% of major programs. It tells you which program to apply for, what documents you need, and even links to the right form. If you’re on Medicare, call the Medicare Rights Center. They help people navigate the Extra Help/PAP gap. If you’re uninsured, contact your local health department. Many have PAP navigators on staff. Don’t assume you don’t qualify. Income limits are higher than you think. And if you’re denied once, try again. Documentation errors are fixable. The right help is out there - you just need to know where to look.Can I get help if I have private insurance?
Usually not - unless your insurance plan has a very high deductible or you’re spending more than $1,000 a month on your medication. Some drug companies now offer “commercial PAPs” for insured patients, but these are limited to specific high-cost drugs like cancer treatments. Always check the manufacturer’s website directly - don’t rely on your insurer’s advice.
What if my income is just above the limit?
Some programs allow exceptions if you have high medical expenses or other financial hardships. Merck, for example, considers applicants who are over the income limit but can prove they can’t afford their meds. You’ll need to submit a hardship letter and documentation like medical bills. It’s not guaranteed, but it’s worth trying.
Do I need to reapply every year?
Yes. Most programs require annual re-enrollment. For specialty drugs like those used for cancer or autoimmune diseases, you may need to re-verify every 3 to 6 months. GSK and Pfizer require updated income documents each time. Missing a deadline means losing your medication - so set calendar reminders.
Can I use a PAP and Medicare Extra Help at the same time?
Yes - but only if you’re approved for Extra Help first. If your income is between 135% and 150% of the Federal Poverty Level, you might be denied Extra Help. In that case, some drug companies (like Takeda) will still help you - but only after you submit proof of your Extra Help denial. This gap affects thousands of people each year.
How long does it take to get approved?
Approval usually takes 10 to 14 days. But if your paperwork is incomplete, it can take weeks longer. The fastest approvals happen when you submit all documents at once: tax return, prescription, doctor’s signature, and proof of residency. Some programs, like Pfizer’s, now use TurboTax integration to speed up income verification - cutting approval time by nearly half.