Leprosy Explained: Causes, Symptoms & Treatment Options

Leprosy Treatment Guide
Leprosy Treatment Guide
This tool helps determine WHO classification and recommended treatment regimen for leprosy based on your symptoms. Remember, only a healthcare professional can diagnose leprosy.
Recommended Treatment
When you hear the word Leprosy is a chronic infectious disease caused by a slow‑growing bacteria that primarily attacks skin and peripheral nerves. Understanding how it spreads, what early signs look like, and how modern medicine can halt its progression is crucial for anyone concerned about this often‑misunderstood illness.
What is Leprosy?
Leprosy (also known as Hansen's disease) is an ancient disease that still affects tens of thousands of people worldwide. The World Health Organization (WHO) estimates that over 200,000 new cases are reported each year, with the majority in South Asia, Africa, and Latin America.
Who or what causes Leprosy?
The culprit is Mycobacterium leprae, a rod‑shaped bacterium that thrives at cooler body temperatures, such as those found in the skin, ears, nose, and superficial nerves. Because the organism divides very slowly-about one cell every 14 days-symptoms can take years to appear after exposure.
Transmission occurs most commonly through prolonged close contact with an untreated person’s nasal droplets. The bacterium does not spread via casual touch or shared objects, which is why stigma often outweighs the actual infection risk.
Who is at risk?
- People living in endemic regions with limited access to health services.
- Individuals with weakened immune systems, such as those with HIV or malnutrition.
- Close household members of an untreated case, especially if living in crowded conditions.
Genetic factors also play a role; certain HLA types appear to increase susceptibility, although research is ongoing.
Recognizing the symptoms
Early signs are often subtle and can be missed for years. Common manifestations include:
- Skin lesions: flat, hairless patches that may be lighter or darker than surrounding skin. They typically feel numb because the underlying nerves are damaged.
- Nerve damage: loss of sensation in hands, feet, or face, leading to injuries that go unnoticed.
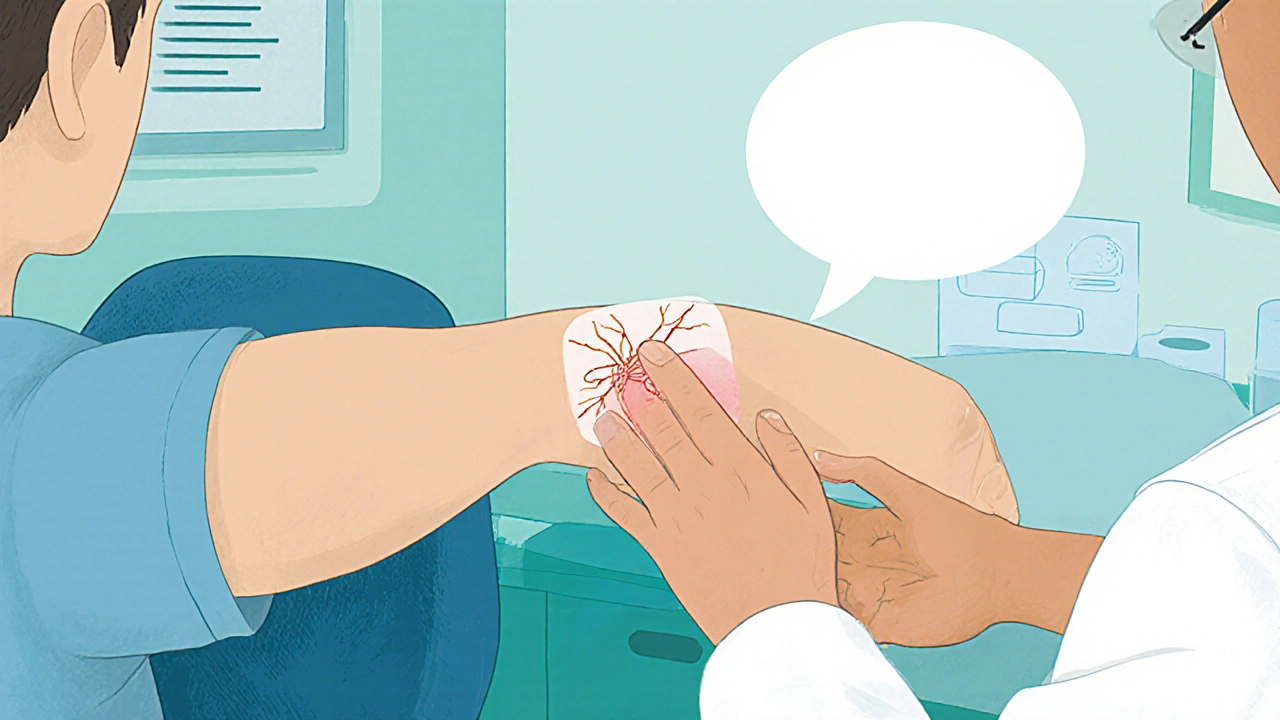
- Thickened peripheral nerves, especially around the elbows, knees, and wrists, which can be felt as firm cords under the skin.
- Muscle weakness and facial droop, giving a characteristic “masked” appearance in advanced cases.
If any of these signs appear and you have lived in or traveled to a leprosy‑endemic area, seeking medical evaluation promptly can prevent permanent disability.
How doctors diagnose Leprosy
Diagnosis combines clinical observation with laboratory confirmation:
- Physical examination of skin lesions and peripheral nerves.
- Skin‑smear test (also called slit‑skin smear): a small sample from a lesion is stained and examined under a microscope for acid‑fast bacilli.
- Skin biopsy: histopathology can reveal granulomas and bacilli, helping to differentiate leprosy from other dermatological conditions.
- Polymerase chain reaction (PCR) testing: increasingly used in reference labs to detect Mycobacterium leprae DNA with high sensitivity.
The WHO classifies leprosy into two main categories for treatment purposes: paucibacillary (1-5 skin lesions) and multibacillary (more than 5 lesions or positive smear). This classification guides the length and composition of therapy.

Treatment options
Since the early 1990s, the global standard has been Multidrug Therapy (MDT), a fixed‑dose combination of three antibiotics that kills the bacteria and prevents resistance.
| Classification | Drugs (monthly dose) | Duration |
|---|---|---|
| Paucibacillary | Dapsone + Rifampicin | 6 months |
| Multibacillary | Dapsone + Rifampicin + Clofazimine | 12 months |
All three drugs are taken under direct observation to ensure adherence. Side effects are generally mild-skin discoloration from clofazimine being the most visible-but routine monitoring is essential.
In addition to antibiotics, managing leprosy reactions is critical. Two types of immune‑mediated reactions can occur during or after MDT:
- Type 1 (reversal) reaction: sudden inflammation of existing lesions and nerves. High‑dose corticosteroids are the mainstay to protect nerve function.
- Type 2 (ENL) reaction: painful nodules, fever, and systemic symptoms. Thalidomide (where not contraindicated) or prolonged steroids are used.
Physical therapy, protective footwear, and education about self‑care help prevent disability after the infection is cleared.
Living with Leprosy: Reducing Stigma and Supporting Recovery
Even with effective treatment, the social impact of leprosy can linger. Stigma often stems from misconceptions that the disease is highly contagious or a moral failing. Public health campaigns by the World Health Organization emphasize that early treatment stops transmission and that most patients lead normal lives.
Community‑based rehabilitation programs provide:
- Occupational therapy to regain hand function.
- Psychosocial counseling to address anxiety and self‑esteem issues.
- Economic support, such as micro‑credit schemes, to reintegrate patients into the workforce.
Family education is equally important; knowing how to care for affected limbs, recognize early signs of nerve damage, and encourage adherence to MDT greatly improves outcomes.
Frequently Asked Questions
Can Leprosy be cured?
Yes. A six‑ to twelve‑month course of MDT cures the infection in more than 95% of cases and stops further transmission.
Is Leprosy contagious?
It spreads through prolonged close contact with an untreated person’s nasal secretions. Casual contact, sharing clothing, or shaking hands does not transmit the disease.
What are the early signs I should watch for?
Look for hairless skin patches that feel numb, unexplained thickened nerves, or a loss of sensation in the hands or feet. Early medical evaluation can prevent nerve damage.
Do I need to isolate myself if I’m diagnosed?
No. Once you start MDT, you are no longer infectious after a few weeks. Maintaining normal social activities is encouraged.
Can leprosy cause permanent disability?
If nerve damage is left untreated, it can lead to permanent loss of sensation, muscle weakness, and deformities. Prompt treatment of reactions and physiotherapy greatly reduce this risk.
Leprosy isn’t something to panic about if you get proper treatment.
India has fought leprosy for centuries and still stands proud-our doctors and community health workers keep the stigma at bay!!! It’s absurd that people still whisper about "contagion" when the science is clear; you only catch it from prolonged close contact with an untreated case!!! We must smash these outdated myths and champion early diagnosis, because our heritage deserves modern, compassionate care!!!
Early detection really does make a huge difference, especially with the MDT regimens that are so effective. Getting checked promptly can stop nerve damage before it becomes permanent. It’s great that the article laid out the symptoms clearly, so folks can recognize those hairless patches and numb areas. If you suspect anything, seeing a health professional right away is the best move.
It is noteworthy that multidrug therapy has transformed leprosy management globally. The combination of dapsone, rifampicin, and clofazimine, administered under direct observation, ensures adherence and prevents resistance. Moreover, the duration-six months for paucibacillary and twelve months for multibacillary-offers a clear treatment timeline. Such protocols, when coupled with vigilant monitoring for reactions, markedly reduce disability rates.
Leprosy is curable with the standard six‑ to twelve‑month MDT course. The WHO guidelines are very clear on dosage and monitoring. Side effects are generally mild, with clofazimine causing skin discoloration in some cases. Physical therapy and protective footwear are essential after bacterial clearance to prevent residual nerve damage.
Excellent summary! Adding a reminder to keep up with follow‑up appointments can help catch any reactions early.
Let’s remember that community support plays a massive role!!! Education campaigns, micro‑credit schemes, and rehabilitation programs empower patients to reintegrate fully!!! The fight against leprosy isn’t just medical-it’s social, cultural, and economic!!!
lol totally agree, the social side is key. Gotta help folks get back to work and stuff.
yeah, plus getting the right shoes and a bit of physio can make a world of difference.
We should encourage more peer‑support groups-it’s amazing how sharing experiences reduces isolation!!! Individuals often feel alone, but connecting with others who’ve walked the same path builds resilience!!!
Honestly, some of these articles sound like they’re trying too hard to be ‘inclusive’ 🙄. The facts are clear, no need for extra fluff 🤷♀️.
Leprosy, also known as Hansen’s disease, has a long history that dates back to ancient times, and its persistence in certain regions highlights gaps in public health infrastructure. The bacterium Mycobacterium leprae prefers cooler parts of the body, which explains why skin lesions and nerve involvement are hallmark signs. Early detection is crucial because the disease progresses slowly, often taking years to manifest clinically, which can lead to delayed diagnosis. Modern diagnostics combine clinical examination with laboratory tests such as skin smears and biopsies, while PCR offers higher sensitivity in specialized labs. Treatment relies on multidrug therapy, a regimen that has proven effective in curing over 95% of patients, reducing both transmission and disability. The standard WHO protocols differentiate between paucibacillary and multibacillary cases, prescribing six months of therapy for the former and twelve months for the latter. Monitoring for leprosy reactions, both type 1 (reversal) and type 2 (ENL), is essential, as these immune responses can cause additional nerve damage if not managed promptly with corticosteroids or thalidomide where appropriate. Rehabilitation services, including physiotherapy and occupational therapy, are vital for restoring function and preventing deformities after bacterial clearance. Social stigma remains a major barrier; education campaigns that emphasize the low contagion risk after treatment can help dismantle misconceptions. Community‑based programs that provide economic support, such as micro‑credit, empower affected individuals to reintegrate socially and financially. Family education on wound care and nerve monitoring further enhances patient outcomes. In summary, while leprosy is curable, comprehensive care must address medical, rehabilitative, and psychosocial dimensions to achieve full recovery and societal inclusion.