How to Verify the Prescriber and Pharmacy Information on Your Medication Label
Every time you pick up a new prescription, you’re holding a safety document - not just a piece of paper with your name and a drug name. The label on your medicine bottle or package is your first and most reliable line of defense against dangerous mistakes. But most people glance at it, grab the pills, and walk out. That’s risky. Prescriber verification isn’t just a suggestion - it’s a life-saving habit.
What You Need to Check on Every Label
When you get your medication, pause for 60 seconds. Don’t rush. Look for these five key pieces of information:
- Prescriber’s full name - This should match exactly who you saw. If your cardiologist prescribed it, the label shouldn’t say "Dr. James Lee, General Practitioner."
- NPI number - A 10-digit number assigned to every licensed provider in the U.S. It’s usually printed near the prescriber’s name. If you’re unsure, call the pharmacy and ask them to confirm it.
- Pharmacy name and address - Make sure it’s the pharmacy you chose. Mail-order pharmacies often send meds from different locations - that’s normal, but you should still recognize the name.
- Pharmacy phone number - This is your direct line to a pharmacist. If something looks off, call this number. Don’t call the prescriber’s office unless you’re told to.
- Prescription number - This number (often labeled "Rx#") is how the pharmacy tracks your refill. Write it down or save it in your phone. You’ll need it every time you call for a refill.
These aren’t just details - they’re your verification checklist. If even one thing doesn’t match what you expect, stop. Don’t take the pills. Call the pharmacy.
Why This Matters: The Real Risks
In 2023, the FDA reported over 1.3 million injuries from medication errors - and 12% of those were tied to incorrect prescriber or pharmacy info. That’s not a small number. It’s not a glitch. It’s preventable.
Here’s what goes wrong:
- Wrong doctor listed - A dentist’s prescription gets auto-filled under your primary care doctor’s name in the system. You take a painkiller meant for a tooth procedure, but you’re on blood thinners. Dangerous mix.
- Wrong pharmacy - Your insurance sends your refill to a different mail-order center than usual. They fill it with a similar-looking drug. You don’t notice until you start feeling sick.
- Misspelled names - "Dr. Chen" becomes "Dr. Chen" or "Dr. Chen". Sounds minor - until you realize the label says a doctor you’ve never seen prescribed your heart medication.
One Reddit user in March 2024 shared how they caught a prescription meant for their mother - the name on the label was their mother’s, but the prescriber was their own doctor. The pharmacy had mixed up two similar-looking patient IDs. That’s the kind of error that kills people.
And it’s not rare. A 2023 study from the Institute for Safe Medication Practices found that 8.7% of wrong-drug errors happened because the prescriber name didn’t match the patient’s records. That’s nearly 1 in 10 errors - all preventable.
Physical Labels Still Beat Apps - Here’s Why
You might think: "Why not just use my pharmacy’s app?" It’s easier, right?
Not always.
A 2023 study in the Journal of the American Pharmacists Association compared physical label checks with app-based verification. The results? Apps had a 7.2% error rate. Physical labels? Just 2.1%. Why? Because apps can glitch. They can show outdated info. They can auto-fill the wrong prescriber. But a printed label? It’s static. It’s real. It’s right in front of you.
That’s why the FDA still recommends checking the physical label - even if you use an app. Use the app as a backup, not your only tool.

Common Problems - And How to Fix Them
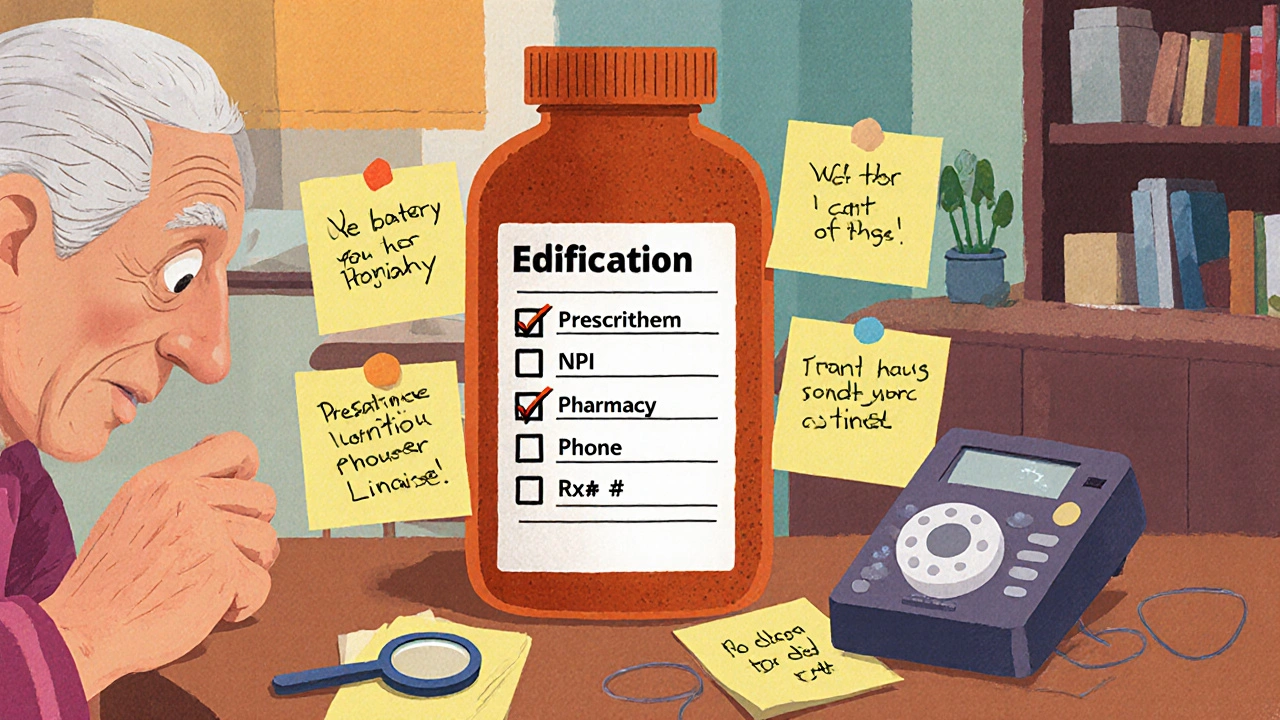
Not everyone sees the label the same way. Here are the top issues patients face - and what to do:
- Small print - 37% of people over 65 struggle to read labels. Solution: Ask the pharmacy for a large-print version. Most pharmacies (82%) have magnifiers or print labels in bigger font for free.
- Hard-to-spell names - "Dr. Srinivasan" or "Dr. O’Connor" - you’re not sure how it’s spelled. Solution: Ask the pharmacist to say it out loud. Write it down. Then compare it to your doctor’s name on your records.
- Electronic prescription errors - 18% of mistakes happen because the system auto-filled the wrong prescriber. Solution: Always compare the label to your appointment notes. Did your oncologist really prescribe this? If not, question it.
- Specialty meds - If you’re getting complex drugs (like for cancer, MS, or rare diseases), the error rate is 23% higher. Solution: Ask for a pharmacist consultation. Most pharmacies offer free med reviews for specialty drugs.
How to Build a Verification Routine
You don’t need to be a medical expert. You just need a habit. Here’s a simple 3-step routine:
- When you pick it up - Check the label right there at the counter. Don’t wait until you get home. If something’s wrong, the pharmacist can fix it on the spot.
- Before you take your first dose - Look at the label again. Compare it to your doctor’s instructions. Is the dose right? Is the name correct? Is the pharmacy familiar?
- When you refill - New bottle? New label? Always check. Even if you’ve taken this drug for years, the prescriber or pharmacy might have changed.
Keep a personal medication record. Write down every drug you take - name, dose, prescriber, pharmacy, and date started. Many pharmacies now offer free digital versions through their apps. Use them. Update them after every refill.
When to Call the Pharmacy - And When to Call Your Doctor
Not every mistake needs a doctor’s visit. Here’s when to call who:
- Call the pharmacy if: the prescriber name is misspelled, the pharmacy address is wrong, the prescription number doesn’t match your records, or the dosage looks off.
- Call your doctor if: you’re unsure if the medication was meant for you, you’re taking multiple drugs and aren’t sure if this one interacts, or the label says the drug is for a condition you don’t have.
Pharmacists are trained to catch errors. They’re your allies. Don’t feel awkward asking questions. In fact, the FDA says patients who ask questions reduce their risk of error by 40%.
What’s Changing in 2025
Things are improving - slowly. In May 2024, the FDA started testing QR codes on labels. Scan it, and you get a digital version of your prescription info - including the prescriber’s license number and a link to verify their credentials. Early results show a 19% increase in accurate verification.
Also, Medicare Part D now requires pharmacies to offer medication reviews for seniors. That means if you’re on Medicare, you can ask for a free one-on-one session with a pharmacist to go over every pill you take.
But here’s the truth: technology helps - but it doesn’t replace you. The FDA’s 2024 report says: "Patient engagement remains the most effective safety tool we have."
Final Check: Your Verification Checklist
Before you swallow your next pill, run through this quick list:
- Is the prescriber’s name spelled right? Does it match who you saw?
- Is the NPI number there? (Ask if you don’t see it.)
- Is the pharmacy name and number correct?
- Does the prescription number match your records?
- Is the dose and instructions what your doctor told you?
If all five say yes - you’re safe. If one says no - stop. Call the pharmacy. Don’t guess. Don’t assume. Your life isn’t worth the risk.
What if the prescriber name on my label doesn’t match my doctor?
Stop. Don’t take the medication. Call the pharmacy immediately. This is one of the most common causes of wrong-drug errors. It could mean the prescription was filled for someone else, or the electronic system mixed up your records. The pharmacy can verify the original prescription and correct the label. If they can’t explain it, contact your doctor’s office.
Can I trust the pharmacy app instead of the physical label?
No - not alone. Pharmacy apps can be inaccurate due to syncing errors, outdated data, or auto-fill mistakes. A 2023 study found physical label checks had a 75% lower error rate than app-based verification. Use the app as a secondary check, but always verify the printed label first.
Why is the NPI number important on my label?
The NPI (National Provider Identifier) is a unique 10-digit number assigned to every licensed healthcare provider in the U.S. It confirms the prescriber is a real, registered professional. If the label doesn’t have it, ask the pharmacy for it. If they can’t provide it, that’s a red flag - the prescription may not be legitimate.
What should I do if I find an error after I’ve already taken a pill?
Call the pharmacy right away. Then call your doctor or go to urgent care. Don’t wait for symptoms. Even if you feel fine, you may have taken the wrong drug or wrong dose. Keep the bottle, label, and packaging - you’ll need them for the pharmacist and doctor to investigate what happened.
Are independent pharmacies more accurate than big chains?
Yes - according to a 2023 survey by Consumer Reports, independent pharmacies scored 4.2/5 for label clarity, while large chains scored 3.7/5. That’s because independent pharmacies often have fewer prescriptions to process and more time to double-check each one. But accuracy is still high at major chains - around 98.7% for prescriber info. The key isn’t which pharmacy you use - it’s whether you verify the label every time.
Just checked my last prescription-turns out my cardiologist’s name was misspelled as ‘Dr. Chenn’ 😳. Called the pharmacy, they fixed it right away. Never skip this step, folks.
So let me get this straight-we’re supposed to treat a pharmacy label like it’s the last will of a dying wizard? 🧙♂️💀 I mean, sure, I’ll check it… but why does my life hinge on whether ‘Dr. O’Connor’ has an apostrophe or not? This feels like a cult.
lol i just glance at the pill color and go. if i dont die in 3 days its fine. 🤷♂️
Y’all are acting like the FDA is your mom and the label is your lunchbox. I’ve been taking metformin for 12 years and my label once said ‘Dr. Satan’ and I still didn’t turn into a demon. Stop being scared of paper.
OMG YES. I used to skip checking labels until my cousin almost took someone else’s blood thinner-same last name, same pharmacy. She ended up in the ER. Now I check every single time, even if it’s the same med I’ve taken for years. It’s not paranoia, it’s peace of mind 💪❤️
Oh my goodness, I love this so much! I’ve been doing this for years, and honestly, it’s changed my life. I write down every prescription, I keep a little notebook next to my pill organizer, I call the pharmacy if something looks even slightly off-even if it’s just the font size. And guess what? I’ve never had a medication error. It’s not hard, it’s just… intentional. And intentionality is the secret sauce of safety. You don’t need to be a doctor-you just need to care enough to pause. And that? That’s heroic.
The NPI validation protocol is critical in mitigating prescriber identity ambiguity within the Rx workflow. Systemic misalignment between EHR and dispensing modules remains a top-tier risk vector. Proactive verification reduces adverse drug events by 40% per ISMP data. Always cross-reference with the prescriber’s credential registry.
Why are we even talking about this? In America, we trust the system. If the pharmacy messes up, sue them. Stop babying people. My grandma didn’t check labels and she lived to 92. You’re overcomplicating medicine.
Okay but… what if you’re blind? Or have severe dyslexia? Or can’t afford glasses? The whole ‘just check the label’ thing sounds great until you realize not everyone can. Maybe the real solution is better accessibility-not just more vigilance from patients who are already overwhelmed.