How to Tell a Side Effect from a True Drug Allergy

Every year, millions of people avoid life-saving medications because they think they’re allergic - but most of them aren’t. You take a pill, get a rash, or feel nauseous, and you assume it’s an allergy. But here’s the truth: drug allergy is rare. Only 5 to 10% of adverse reactions are true allergies. The rest? Side effects. And mistaking one for the other can cost you more than just a headache - it can cost you your health.
What’s the Real Difference?
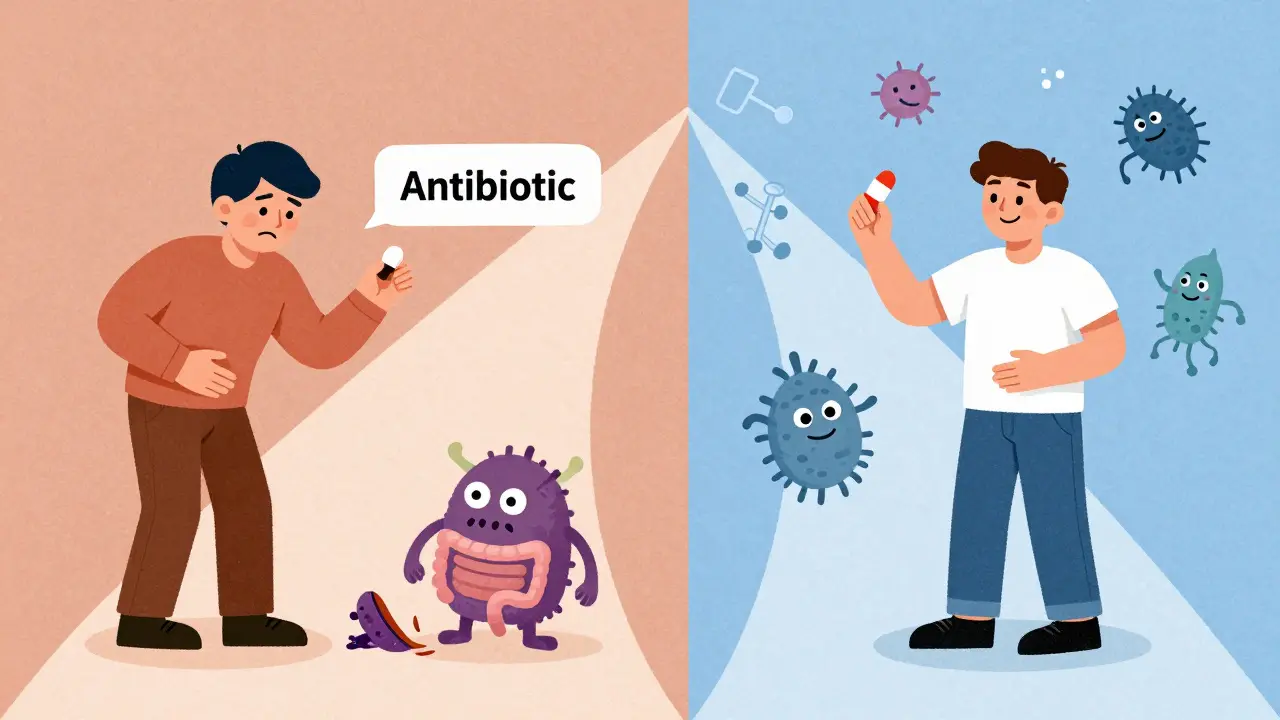
A drug allergy is your immune system going into overdrive. It sees the medication as an invader and attacks it. That triggers real immune responses - swelling, hives, trouble breathing, even anaphylaxis. These reactions happen because your body produces specific antibodies, like IgE, that recognize the drug as dangerous. Once that happens, every future exposure can be worse. A side effect is just your body reacting to the drug’s chemistry. It’s not your immune system. It’s the drug doing what it’s supposed to do - but in the wrong place. For example, antibiotics kill bacteria, but they also mess with your gut flora. That’s why you get diarrhea. Painkillers reduce inflammation, but they also irritate your stomach lining. That’s why you get nausea. These reactions are predictable, dose-dependent, and often fade if you keep taking the drug or lower the dose.Timing Tells the Story
When did the reaction happen? That’s your first clue. If you got hives, swelling, or trouble breathing within minutes to an hour after taking the drug, that’s a classic sign of an allergic reaction. IgE-mediated allergies strike fast. Think: you took amoxicillin, and 20 minutes later, your face puffed up and your throat felt tight. That’s not a side effect. That’s an emergency. But if you started feeling dizzy or nauseous after a few hours - or even days - that’s more likely a side effect. Some delayed reactions, like a rash that appears 7 to 14 days after starting a drug, can still be allergic (T-cell mediated), but they’re not the same as the immediate, life-threatening kind. Severe delayed reactions like DRESS or Stevens-Johnson Syndrome are rare but dangerous. They require stopping the drug immediately and seeing a specialist.Symptom Patterns Are Key
Allergies don’t stick to one system. They spread. If you only have nausea? Probably a side effect. Only a headache? Likely a side effect. But if you have a rash and swelling and trouble breathing? That’s an allergic reaction. The Mayo Clinic found that 87% of true drug allergies involve two or more body systems at once. Side effects? Usually just one. Here’s what to watch for:- True allergy signs: Hives (raised, itchy welts), angioedema (deep swelling under skin), wheezing, low blood pressure, vomiting with skin rash, throat tightness.
- Side effect signs: Nausea, dizziness, dry mouth, constipation, fatigue, mild stomach upset - especially if they match the drug’s known profile.
Penicillin: The Most Misunderstood Allergy
About 7% of Americans say they’re allergic to penicillin. That sounds like a lot. But here’s the shocking part: 90 to 95% of them aren’t. They had nausea or diarrhea after taking it as a kid. Or a mild rash that turned out to be a virus. Or they were told they were allergic without testing. Now, they’re stuck with stronger, costlier, less effective antibiotics - and they’re more likely to get dangerous infections like C. diff. A 2022 JAMA study showed people with false penicillin allergies had 69% higher rates of C. diff and stayed in the hospital 30% longer. That’s not just inconvenient - it’s deadly. The good news? You can get tested. Skin tests and oral challenges are safe, accurate, and done in controlled settings. If you think you’re allergic to penicillin, ask your doctor about getting evaluated. You might be able to take it again.What Happens When You Get It Wrong?
Mislabeling a side effect as an allergy has real consequences. Doctors avoid the drug you “can’t take.” They prescribe something else - often a broader-spectrum antibiotic like vancomycin or clindamycin. These drugs are more expensive. They kill more good bacteria. They increase your risk of superbugs. The CDC estimates false penicillin allergy labels cost the U.S. healthcare system over $1 billion a year. And it’s not just antibiotics. If you think you’re allergic to ibuprofen because you got a headache, you might avoid all NSAIDs. That limits your pain options. If you think you’re allergic to aspirin because you got a stomach ache, you might miss out on heart protection.How Do Doctors Know for Sure?
There’s no blood test you can buy online that will tell you if you’re allergic. Diagnosis requires expertise. For immediate reactions (like hives or anaphylaxis), doctors use skin testing. A tiny amount of the drug is placed under your skin. If you react, it’s an allergy. For penicillin, this test is 95% accurate. For delayed reactions, patch tests or lymphocyte tests are used. These take longer but help identify T-cell mediated allergies. Sometimes, a controlled drug challenge is the only way to know. You’re given a small, increasing dose of the drug under supervision. If nothing happens, you’re cleared. This is how 92% of patients at Mayo Clinic are successfully de-labeled.
What You Should Do
If you think you have a drug allergy, here’s what to do:- Write it down. When did it happen? What were you taking? What exactly happened? How long did it last? Don’t rely on memory - write it the day it happens.
- Don’t assume. Nausea isn’t an allergy. Dizziness isn’t an allergy. A mild rash that fades? Maybe not.
- Ask for testing. If you were told you’re allergic to penicillin or another common drug, ask your doctor if you can be evaluated. Most people can safely take the drug after testing.
- Update your records. If you’re cleared, make sure your EHR (electronic health record) is updated. Many hospitals now have pharmacist-led allergy review programs.
What’s Changing in 2026
The FDA now requires drug labels to clearly separate side effects from allergies. Electronic health records must distinguish between the two in structured data fields - a rule that went fully into effect in January 2025. New tools are helping. Epic Systems’ Allergy Assessment Module uses AI to flag patients with likely false allergy labels and prompts doctors to refer them for testing. Hospitals with these programs are seeing a 35% improvement in accurate classification. And the language is changing. The American College of Allergy, Asthma, and Immunology will soon officially use three terms:- Allergy: Immune-mediated, potentially life-threatening.
- Intolerance: Non-immune adverse reaction - uncomfortable, but not dangerous.
- Side effect: Expected, known pharmacological effect.
i just took amoxicillin last week and got a tiny rash... now i’m terrified i’m gonna die in my sleep 😭 also why does everyone assume we’re dumb enough to not know the difference between side effects and allergies? like i read the pamphlet, i swear.
This is actually one of the most important public health issues no one talks about. I’m a pharmacist and I see this daily. People get labeled allergic to penicillin based on a stomach ache at age 8, then spend the rest of their lives on broader-spectrum antibiotics that wipe out their gut biome, increase C. diff risk, and cost the system thousands. The real tragedy? Most of these people could be safely re-challenged. The testing is safe, quick, and covered by insurance. But doctors don’t bring it up because they’re overworked and patients don’t ask because they’ve internalized the label as fact. It’s a systemic failure wrapped in medical myth.
i had a rash after sulfa drugs in college. thought i was allergic. turned out it was a virus i had at the same time. never got tested. just avoided anything that sounded like it might be related. now i’m 42 and my doc just told me i could’ve taken it fine. kinda mad at my past self for being scared.
The pharmaceutical industry benefits from perpetuating false allergies. More prescriptions for expensive alternatives. More profit. Less accountability. The FDA's new labeling rules are cosmetic. Real change requires dismantling the profit-driven structure of modern medicine.
OMG I’M SO GLAD THIS EXISTS. I’ve been screaming into the void for years that ‘allergic to ibuprofen’ is often just ‘got a headache from ibuprofen’. I had a legit anaphylaxis reaction to penicillin at 12 - got tested at 30 and was cleared. My doctor was shocked I’d never been re-evaluated. Now I take Advil without fear and my stomach doesn’t hate me anymore. Please, if you think you’re allergic - GET TESTED. It’s not just about convenience, it’s about survival.
i used to think if i felt weird after a pill it was an allergy, you know? but then my grandma told me she got dizzy on blood pressure meds for 20 years and finally asked her doc - turns out it was just the timing of when she took it. she started taking it with food and boom, no more dizziness. it’s wild how many things are just about how you use it, not the drug itself. i’m gonna ask my doc about my ‘allergy’ to aspirin now. maybe i just need to take it with a snack 😊
Allergies are a myth created by fear and bad science. Your immune system doesn’t work like that. Everything is a side effect. The system just needs scapegoats to keep people docile. Penicillin? Just a toxin. Your body reacts. That’s not allergy. That’s biology. Stop believing in medical fairy tales.
The T-cell mediated delayed hypersensitivity reactions like DRESS and SJS are underrecognized in primary care. Most clinicians default to IgE-mediated paradigms, which leads to underdiagnosis of non-IgE pathways. This creates a diagnostic blind spot that contributes to iatrogenic harm. We need better training in pharmacovigilance at the residency level.
I had a patient last month who avoided all NSAIDs because she thought she was allergic after a rash at 14. Turned out it was poison ivy. She’d been taking Tylenol for everything for 25 years - even though she had arthritis. We did a challenge. She took naproxen. No reaction. She cried. Said she finally felt like she could live again. That’s the real cost of these labels.
In India, this is even worse. People self-diagnose allergies based on Ayurvedic interpretations or WhatsApp forwards. ‘Aspirin causes heat in the body’ - so they avoid it even for heart attacks. No testing. No education. Just cultural myths layered on top of medical ignorance. The FDA’s new rules won’t fix this unless we invest in global health literacy.
So what you’re saying is we’re all just stupid and the doctors are gods? That’s rich. If you’re so sure about this, why do you think they didn’t test you before? Why do you think the labels stick? Because the system wants you afraid. Don’t fall for the hype.
i got a rash after cipro once and now i avoid all antibiotics like theyre cursed. but honestly i dont even know what a rash looks like anymore. is it red? itchy? does it glow? i just know i felt weird and now i panic. maybe i need to stop being a coward and get tested
The distinction between allergy and intolerance is not merely semantic. It is epistemological. To conflate the two is to risk the erosion of clinical precision and the normalization of diagnostic ambiguity. One must maintain ontological clarity in the face of pharmacological uncertainty.