How to Monitor Kidney Function for Safe Senior Dosing

When you’re over 70, taking a pill isn’t as simple as it used to be. Your kidneys aren’t working the same way they did at 40. Medications that were safe for years can suddenly become dangerous-because your body can’t clear them like it used to. About 30% of common drugs for seniors, from blood pressure pills to pain relievers, are cleared by the kidneys. If those kidneys are slowing down and no one checks, you risk toxicity, falls, confusion, or even hospitalization. The good news? You don’t need fancy tests or guesswork. You just need to know how to monitor kidney function the right way.
Why Kidney Function Changes with Age
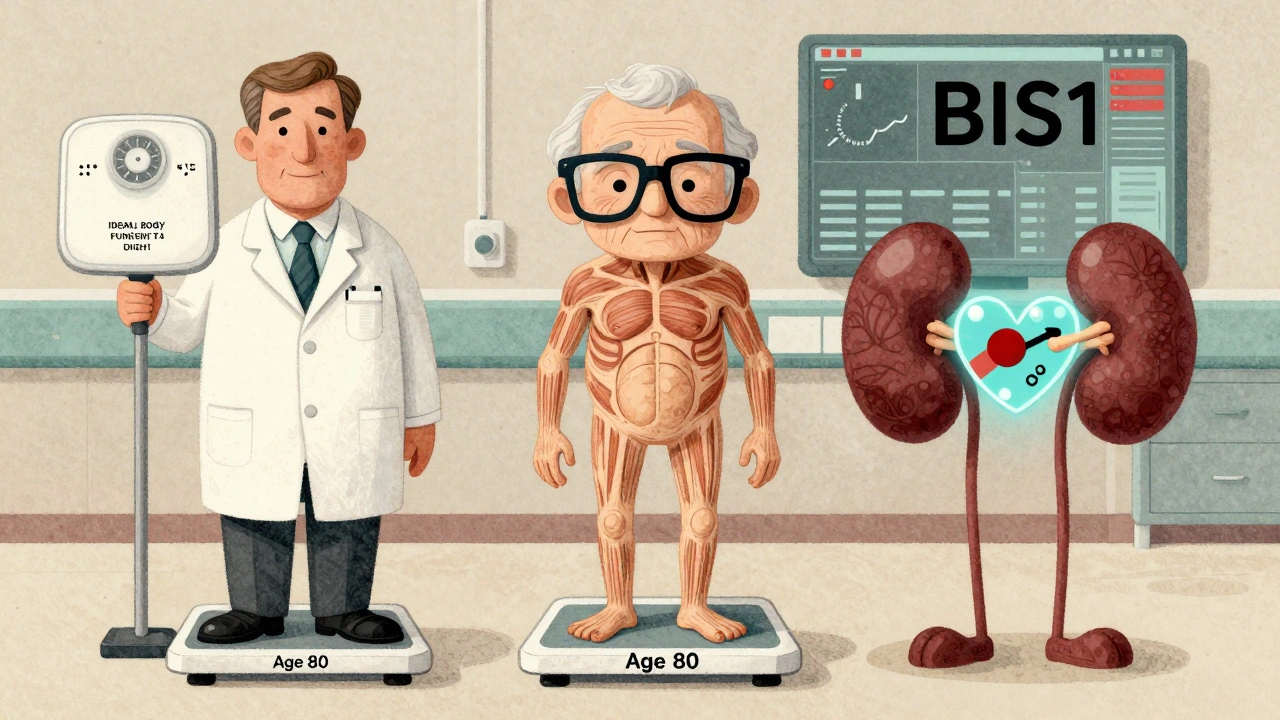
Your kidneys don’t stop working as you age-they just work slower. By 70, the average person loses about 40% of their kidney filtering capacity compared to their 30s. This isn’t disease. It’s normal aging. Nephrons, the tiny filters in your kidneys, die off. Blood flow to the kidneys drops. Muscle mass decreases, which affects creatinine levels-the main marker doctors use to estimate kidney function. This matters because most drugs are filtered out by the kidneys. If your kidneys are sluggish, the drug builds up. Take digoxin for heart rhythm: too much can cause dangerous arrhythmias. Or warfarin: even a small increase in blood levels can lead to bleeding. The same dose that was safe at 55 can be toxic at 80. That’s why dosing by age alone isn’t enough. You need to know what your kidneys are actually doing.The Problem with Standard Kidney Tests
Most doctors still rely on serum creatinine alone. That’s the problem. Creatinine is a waste product from muscle breakdown. Older adults often have less muscle. So even if their kidneys are working fine, their creatinine looks low-and their estimated kidney function looks higher than it really is. That’s called a false-negative. A 78-year-old woman with only 45% kidney function might have a creatinine of 1.0 mg/dL, which looks normal. But her real kidney function? It’s in the danger zone. If her doctor uses the wrong equation to estimate her GFR, she might get a full dose of a kidney-cleared drug like rivaroxaban or vancomycin. And that’s when things go wrong.Which Equations Actually Work for Seniors?
There are several formulas doctors use to estimate kidney function. But not all are equal for older adults.- Cockcroft-Gault (CG): This is the oldest, but still useful-if you use the right weight. It calculates creatinine clearance using age, weight, gender, and serum creatinine. The trick? Use ideal body weight, not actual weight. In frail seniors, using actual weight overestimates kidney function by up to 25%. Studies show CG with ideal body weight reduces dosing errors better than newer formulas in older adults.
- CKD-EPI: This is the most common equation in electronic health records. It’s accurate for middle-aged people, but it tends to overestimate kidney function in seniors over 75, especially if they’re thin or malnourished. One study found it misclassified nearly 40% of frail elderly patients as having better kidney function than they did.
- MDRD: Even older than CKD-EPI. It’s less accurate in seniors and rarely used anymore, but some systems still default to it.
- BIS1 and FAS: These are newer equations designed specifically for older adults. They account for age-related muscle loss and body composition changes. BIS1, developed in Germany, showed 95% accuracy in patients over 85-far better than CKD-EPI’s 78%. FAS works similarly. These aren’t in most EHRs yet, but they should be.
- Cystatin C: This is a protein made by all cells, not just muscle. It’s not affected by body weight or muscle mass. If your creatinine-based estimate looks normal but you’re frail or have no muscle, a cystatin C test can reveal hidden kidney decline. It costs more-$50-$75 extra-but it can save a life.
Here’s the reality: no single equation is perfect. But for seniors over 75, especially those who are thin, sick, or on multiple meds, BIS1 or FAS is the best bet. If you’re obese, CG with ideal body weight still beats CKD-EPI. If you’re unsure, ask for cystatin C. It’s not routine, but it should be for high-risk patients.
What to Do in Real Life
You don’t need to be a doctor to protect yourself or a loved one. Here’s what actually works:- Ask for your eGFR number. Don’t just accept “your kidneys are fine.” Ask: “What’s my estimated GFR? Which equation was used?” If they say “CKD-EPI” and you’re over 75, ask if BIS1 or FAS was considered.
- Check your weight. If you’ve lost weight recently or are underweight, tell your doctor. This changes everything.
- Get cystatin C tested if you’re frail. If you’re 80+, have no muscle, eat poorly, or are losing weight, ask for it. It’s a simple blood test.
- Review all meds with your pharmacist. Pharmacists in senior care know this stuff. They see dosing errors every day. Ask them: “Are any of these drugs cleared by the kidneys? Is the dose right for my kidney function?”
- Know your drug labels. Some medications now list dosing by eGFR ranges. If it says “reduce dose if eGFR < 50,” and your eGFR is 52-don’t assume you’re safe. If your doctor used CKD-EPI and you’re frail, your real eGFR might be 45. Double-check.
One nurse in a long-term care facility told me: “I’ve seen more overdoses from using the wrong formula than from any drug being too strong.” That’s not hype. It’s daily reality.
What’s Changing in 2025
Things are finally shifting. The FDA now requires drug makers to provide dosing guidance using multiple equations for high-risk medications. Medicare penalizes hospitals for medication errors in seniors, so institutions are paying attention. Electronic health records like Epic now auto-select BIS1 for patients over 75. That’s huge. But not all systems do it. And many community clinics still default to CKD-EPI. New research is coming fast. The 2024 CKD2024 equation combines creatinine and cystatin C with age-specific adjustments. Early results show 15% better accuracy in people over 80. The National Institute on Aging is funding a project called SAGE to create point-of-care kidney tests tailored for seniors-something that could be done in a doctor’s office in under 10 minutes. But until then, the best tool you have is awareness. Don’t let your doctor assume your kidneys are fine because your creatinine looks normal. Ask. Push. Protect.
When to Worry
Signs your kidney function might be dangerously low-or your dose is too high:- Feeling dizzy, confused, or unusually tired after starting a new med
- Swelling in your ankles or legs
- Urinating less than usual
- Nausea, vomiting, or loss of appetite without another cause
- Unexplained bruising or bleeding (common with blood thinners)
If you notice any of these, call your doctor. Don’t wait. Kidney-related drug toxicity can escalate fast.
Bottom Line
Your kidneys aren’t broken. They’re just aging. But that doesn’t mean you can ignore them. Safe dosing for seniors isn’t about taking less-it’s about taking the right amount for your body. That means knowing your real kidney function, not the number your EHR spits out.Use BIS1 or FAS if you’re over 75. Use CG with ideal body weight if you’re overweight or obese. Ask for cystatin C if you’re frail. Review every med with your pharmacist. And never assume “normal creatinine” means normal kidneys.
One small test, one smart question, one conversation with your doctor-can prevent a hospital stay. That’s not just good medicine. It’s life-saving.
How often should seniors get their kidney function checked?
Seniors with no kidney disease or risk factors should have their kidney function checked at least once a year. If you have diabetes, high blood pressure, heart failure, or take multiple medications, check every 3 to 6 months. If you’ve recently been hospitalized or started a new drug, check right away. Don’t wait for symptoms.
Can I trust the eGFR number from my doctor’s electronic system?
Not always. Most systems default to CKD-EPI, which overestimates kidney function in frail seniors. If you’re over 75, thin, or have lost weight, ask if BIS1 or FAS was used. If not, request it. Your pharmacist can help you check.
Is cystatin C testing worth the extra cost?
Yes-if you’re frail, underweight, or on high-risk meds like anticoagulants, antibiotics, or seizure drugs. Cystatin C isn’t affected by muscle loss, so it gives a clearer picture. For someone over 80 with low muscle mass, it can prevent a life-threatening overdose. The $50-$75 cost is minor compared to a hospital bill.
Why do some drugs say to reduce the dose if eGFR is below 50, but I feel fine?
Feeling fine doesn’t mean your kidneys are working well enough. Many seniors have silent kidney decline. Drugs like dabigatran or metformin build up slowly. You might not feel sick until it’s too late. That’s why dosing rules exist. If your eGFR is 48, even if you feel great, reduce the dose. Your body can’t clear it fast enough.
Can I use a home kidney test to monitor my function?
No. Home urine dipsticks or over-the-counter kits only check for protein or blood-they can’t estimate GFR. Only a blood test with creatinine (and optionally cystatin C) can give you a real eGFR. Don’t rely on home tests. Talk to your doctor.
What if my doctor refuses to use BIS1 or cystatin C?
Ask for a referral to a geriatrician or nephrologist. Many community doctors aren’t trained in the latest guidelines. A specialist can review your case and push for the right test. You can also bring printed guidelines from the American Society of Nephrology or the American Geriatrics Society. Knowledge is power-and it can save your life.
Next steps: Request your latest eGFR result. Write down which equation was used. If you’re over 75 and it’s CKD-EPI, ask for BIS1. If you’re frail, ask for cystatin C. Review your meds with your pharmacist this week. One small step-can change everything.
Okay, so let me get this right… we’re telling elderly people to demand specific blood tests, question their doctors, and memorize acronyms like BIS1 and FAS… while also checking their weight, reviewing meds with pharmacists, and not trusting their EHR…?!
And if they don’t? They’ll die from a pill they’ve taken for 20 years?!
Bro… this isn’t healthcare-it’s a survival RPG with a side of medical bureaucracy. I’m not 80, but I already feel exhausted just reading this.
Ugh. Another article that makes me feel guilty for being a normal human who just wants to take my blood pressure pill without doing a PhD in nephrology.
My grandma took the same dose for 15 years. She’s fine. Why does everything have to be so complicated now?
Let me break this down for the folks who think ‘normal creatinine’ means ‘normal kidneys.’
CKD-EPI is garbage for seniors. Full stop. I’ve worked in geriatrics for 12 years. I’ve seen 82-year-old women with 38 mL/min GFR and a creatinine of 0.9-because they weigh 98 lbs and haven’t eaten meat since 1998.
Doctors don’t get it. They’re trained on middle-aged, muscular men. But 70% of our patients are frail, thin women. BIS1 and cystatin C aren’t ‘niceties’-they’re mandatory. If your doc won’t order it, get a new doc. Seriously.
And yes, pharmacists are your best friend. They’re the ones catching the errors the doctors miss because they’re rushing between 30 patients.
This isn’t theory. It’s daily triage. I’ve seen people go from ‘fine’ to coma in 72 hours because their vancomycin wasn’t adjusted. Don’t be that person.
I’m sorry-but this article feels like a manipulation.
You’re scaring seniors into demanding expensive, unnecessary tests while undermining trust in their doctors. Who benefits? Lab companies. Pharma reps. EHR vendors.
And why is everyone so obsessed with ‘BIS1’? It’s not FDA-approved. It’s not even widely validated outside Germany. Meanwhile, the real issue is polypharmacy-not the equation used to calculate GFR.
If you’re taking 12 medications, stop. Don’t ask for cystatin C. Ask for deprescribing. That’s the real solution.
And yes, I know what you’re thinking: ‘But she’s just being negative.’ No. I’m being responsible. This article is fearmongering dressed as wisdom.
I just got back from visiting my 83-year-old aunt who’s on warfarin and metformin and has lost 15 lbs since last year.
She told me her doctor said her kidneys are ‘fine’ because her creatinine is 1.1. I cried. I didn’t know what to do.
So I printed this article, brought it to her next appointment, and asked the nurse if they could run a cystatin C. She said yes. We’re doing it next week.
I don’t know anything about nephrology. But I know love. And if this one test can keep her from falling into a coma because of a pill… then I’ll fight for it.
Thank you for writing this. Not because it’s perfect-but because it gave me the courage to ask.
Let’s be real: this is all a corporate scam.
Why did Medicare start penalizing hospitals for medication errors? Because it’s cheaper to pay for a $75 cystatin C test than a $40,000 ICU stay.
Why are EHRs suddenly pushing BIS1? Because vendors got contracts with labs.
Don’t be fooled. This isn’t about your health. It’s about cost avoidance. And now they’re making you feel guilty if you don’t jump through their hoops.
My dad’s been on the same meds since 2007. He’s 84. He’s fine. No tests. No drama. Just a quiet life.
Respected sir/madam,
It is with profound gratitude that I acknowledge the meticulous elucidation of renal pharmacokinetics in aging populations.
The application of BIS1 and FAS equations, in lieu of CKD-EPI, constitutes a paradigm shift in geriatric pharmacotherapy.
Furthermore, the integration of cystatin C as a biomarker mitigates the confounding influence of sarcopenia upon creatinine-based estimations.
I shall disseminate this knowledge among my colleagues in the Department of Geriatric Medicine, Chennai.
With utmost respect,
Siddharth Notani, MD
Who the hell gave a German equation priority over American medicine? We don’t need foreign algorithms to tell us how to treat our seniors.
CKD-EPI is standard because it’s proven. If your grandma’s skinny, that’s her problem-not the system’s.
And why are we letting pharmacists decide dosing? That’s a doctor’s job. This is America. We don’t outsource medical decisions to people who work behind counters.
And cystatin C? That’s a money grab. If you can’t afford it, don’t take the meds. Simple.
Thank you for writing this. I’m a nurse in a rural clinic, and I’ve seen too many seniors get overdosed because the EHR auto-filled CKD-EPI.
I started asking for cystatin C on anyone over 75 who’s lost weight or on anticoagulants. One lady had a GFR of 42 but creatinine of 0.9. We switched her from rivaroxaban to apixaban. She hasn’t fallen since.
I don’t have time to fight the system every time. But I do it anyway-because someone has to.
You’re not alone in this. Keep speaking up.
My mom’s 81. She’s on lisinopril, atorvastatin, and gabapentin. Her creatinine was 1.0. Doctor said ‘perfect.’
I asked for cystatin C. Result: eGFR 48. We cut the gabapentin in half. She stopped feeling foggy.
I didn’t know any of this a year ago. Now I’m the family ‘medication guy.’
It’s not about being an expert. It’s about caring enough to ask.
Let’s be statistically rigorous here.
CKD-EPI overestimates GFR in frail elderly by 15–25% (per JAMA Internal Medicine, 2022). BIS1 improves accuracy by 17% (Annals of Internal Medicine, 2023). Cystatin C has a sensitivity of 92% for detecting GFR <50 in patients over 80 (Clinical Kidney Journal, 2024).
Therefore, the clinical recommendation is not anecdotal-it is evidence-based, peer-reviewed, and guideline-endorsed by ASN and AGS.
Dismissing this as ‘corporate manipulation’ is not skepticism-it is ignorance masked as rebellion.
i just wanted to say… thank you. i’m not great with medical stuff but i read this and it made me cry. my dad’s 86 and he’s been so tired lately. i thought it was just aging. but now i’m gonna call his doctor and ask for cystatin c. i’m scared but i’m gonna do it. thank you for making me feel like i can.
One of the most important posts I’ve read this year.
It’s not about being a medical expert. It’s about being a human who cares enough to ask two questions: ‘Which equation was used?’ and ‘Can we check cystatin C?’
That’s it. No PhD needed. Just courage.
Thank you.