Hormone Therapy for Breast Cancer: Tamoxifen vs Aromatase Inhibitors Explained
What Is Hormone Therapy for Breast Cancer?
Not all breast cancers are the same. About 7 out of 10 breast cancers are fueled by estrogen - these are called hormone receptor-positive cancers. For these cases, hormone therapy isn’t just an option; it’s often the most effective way to stop the cancer from coming back after surgery or radiation. Two main types of drugs are used: tamoxifen and aromatase inhibitors. They work differently, help different groups of women, and come with very different side effects.
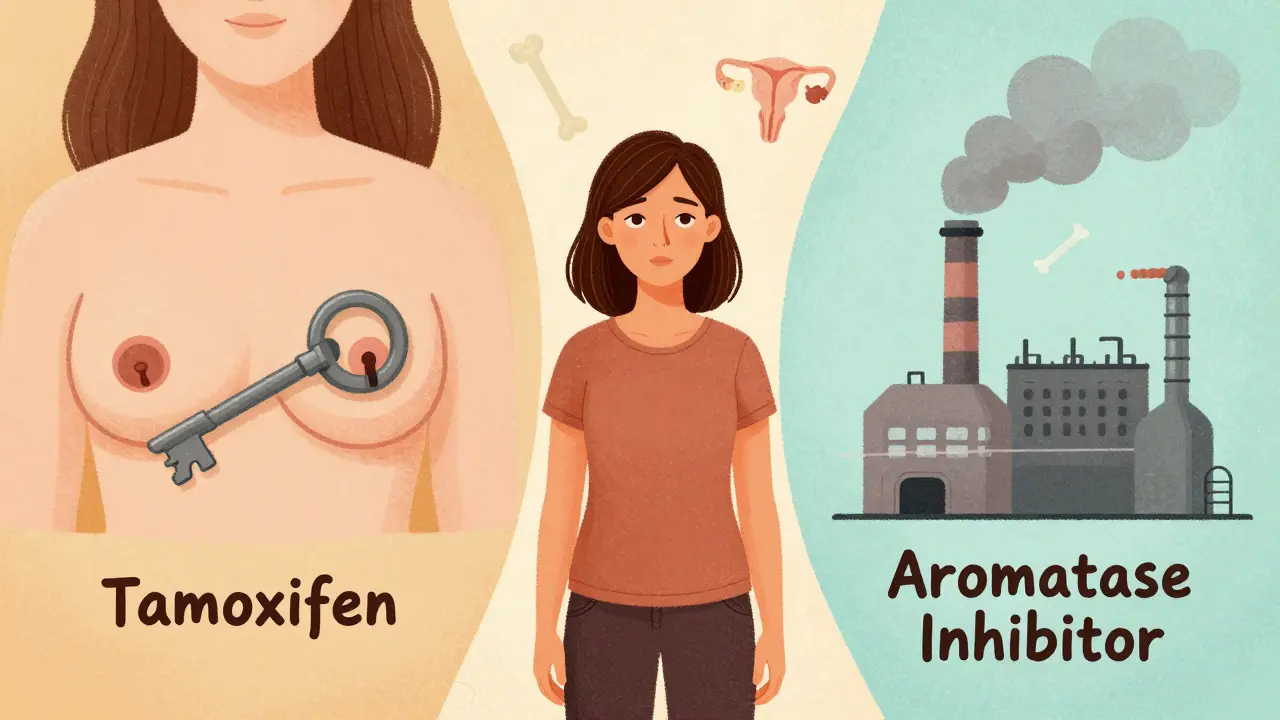
Think of it like this: estrogen is food for these cancer cells. Tamoxifen acts like a fake key that blocks the lock so estrogen can’t get in. Aromatase inhibitors shut down the factory that makes estrogen in the first place. The choice between them isn’t about which is ‘better’ - it’s about which one fits your body, your life, and your risk level.
Tamoxifen: The Long-Standing Option
Tamoxifen has been around since the 1970s. It’s not new, but it’s still essential. It’s a selective estrogen receptor modulator (SERM), meaning it blocks estrogen in breast tissue while allowing it to work elsewhere - like in bones and the uterus. That’s why it’s still the go-to for women who haven’t gone through menopause.
Doctors usually prescribe 20 mg daily, taken as a pill. It stays active in your system for days after you stop taking it, which means even if you miss a dose now and then, it’s not an emergency. But it’s not without trade-offs. About 1 in 10 women on tamoxifen develop thickening of the uterine lining, which raises the risk of endometrial cancer. The chance is small - about 1.2% over 10 years - but it’s real. Blood clots are another concern; the risk of a pulmonary embolism is nearly double compared to aromatase inhibitors.
On the upside, tamoxifen protects bone density. For younger women, that’s huge. Many women report hot flashes and mood swings, but those often settle down after the first year. And unlike aromatase inhibitors, tamoxifen doesn’t cause joint pain in most people. For women who can’t tolerate bone loss or joint pain, tamoxifen might be the only option that lets them stay on treatment long-term.
Aromatase Inhibitors: The Modern Alternative
Aromatase inhibitors (AIs) - like anastrozole, letrozole, and exemestane - came into wide use in the early 2000s. They work by blocking the aromatase enzyme, which turns male hormones into estrogen in fat tissue. In postmenopausal women, this is the main source of estrogen. AIs cut estrogen levels by 95% or more.
Studies show they’re more effective than tamoxifen at preventing recurrence in postmenopausal women. In one major trial, women on letrozole had a 30% lower chance of cancer returning compared to those on tamoxifen. Over 10 years, this meant 2.1% fewer deaths from breast cancer. That’s not just a number - it’s one extra woman alive for every 48 treated.
But the cost is physical. About half of women on AIs report joint and muscle pain - sometimes so bad they can’t lift a coffee cup or walk up stairs. Bone thinning is common. About 6.4% of women on AIs break a bone within 10 years, compared to 5.1% on tamoxifen. That’s why doctors start DEXA scans right away. If your bone density drops too far, you’ll be put on drugs like zoledronic acid or denosumab to protect your skeleton.
Some women also report brain fog or memory issues, though this is harder to prove. One survey found nearly half of AI users felt their ‘chemo brain’ got worse. Still, many appreciate that AIs don’t raise the risk of uterine cancer. If you’ve had a history of blood clots or are at high risk for endometrial cancer, AIs are often the safer choice.

Who Gets Which Drug?
It’s not complicated: if you’re premenopausal, you get tamoxifen. If you’re postmenopausal, you get an aromatase inhibitor. That’s the rule - but there are exceptions.
For younger women with higher-risk cancer, doctors now add ovarian suppression. That means using shots like goserelin to turn off the ovaries and make you temporarily menopausal. Then, you can add an AI. The TEXT and SOFT trials showed this combo reduces recurrence by 21% compared to tamoxifen alone. For a woman with aggressive cancer, that’s worth the extra side effects - but it’s not for everyone.
For older women, especially those with mild, slow-growing tumors, tamoxifen might still be preferred. Why? Because AIs increase fracture risk, and older women are already at higher risk for falls and broken hips. One study showed that for a 70-year-old woman with low-risk cancer, the extra benefit of an AI might not outweigh the risk of a hip fracture.
Genetic testing also plays a role. Tamoxifen needs to be processed by the CYP2D6 enzyme to become active. About 7% of people have a genetic variation that makes them poor metabolizers. For them, tamoxifen may not work as well. If you’re a poor metabolizer and you’re premenopausal, your doctor might still recommend tamoxifen but add closer monitoring. If you’re postmenopausal, you’re better off on an AI anyway.
How Long Do You Take It?
Most women take hormone therapy for five years. That’s the standard. But for some, five years isn’t enough.
If your cancer was large, spread to lymph nodes, or had high-grade features, you might be offered up to 10 years. The MA.17X trial showed that extending AI therapy from 5 to 10 years reduced recurrence by another 3%. But the side effects keep piling up. More joint pain. More bone loss. More fatigue. So the decision isn’t just medical - it’s personal.
Some women switch halfway through. Start with tamoxifen for 2-3 years, then switch to an AI. Studies show this gives the same protection as starting with an AI from day one. It’s a smart middle ground: you get the bone protection of tamoxifen early on, then the stronger cancer-fighting power of an AI later.
For low-risk patients, new trials are asking if three years is enough. The PERSEPHONE trial is testing whether shorter treatment works just as well. If it does, it could mean fewer side effects and lower costs - especially important in places where AIs cost $150 a month and tamoxifen is $15.
Real-Life Trade-Offs
Real people make real choices based on real symptoms. On online forums, women talk about the daily grind of side effects. One woman wrote: ‘I chose tamoxifen because I didn’t want to be in pain every day. I can handle hot flashes - I can’t handle not being able to open a jar.’ Another said: ‘I’d rather have joint pain than worry about my uterus bleeding again.’
Surveys show that 68% of AI users report moderate to severe joint pain. About 22% stop treatment because of it. For tamoxifen users, only 8% quit due to side effects. But 63% of tamoxifen users say hot flashes are their biggest problem - worse than any AI side effect.
One study found that 72% of tamoxifen users were happy with their choice because their bones stayed strong. Meanwhile, 78% of AI users felt relieved they didn’t have to worry about uterine cancer. Neither drug is perfect. The best choice is the one you can live with for five to ten years.
What’s Next in Hormone Therapy?
The field isn’t standing still. In 2023, the FDA approved camizestrant, a new oral drug called a SERD - selective estrogen receptor degrader. It doesn’t just block estrogen like tamoxifen or shut it down like AIs. It destroys the estrogen receptor entirely. Early results show it cuts recurrence by 38% in women with a specific genetic mutation (ESR1). This is the first major advance since aromatase inhibitors.
Doctors are also moving toward personalized treatment. Genomic tests like Oncotype DX tell you how likely your cancer is to come back. If your score is low, you might not need chemo at all - and hormone therapy alone might be enough. That changes how long you need to take it, and whether you need the strongest option.
For now, tamoxifen and aromatase inhibitors remain the backbone of treatment. But the future is clearer: fewer one-size-fits-all plans, and more decisions based on your genetics, your risk, and your life.
What Should You Do?
Don’t just accept the first recommendation. Ask your doctor:
- Is my cancer hormone receptor-positive?
- Am I pre- or postmenopausal?
- What’s my risk of recurrence - low, medium, or high?
- Do I have a history of blood clots, uterine issues, or osteoporosis?
- What are my biggest concerns: hot flashes, joint pain, or cancer coming back?
There’s no perfect drug. But there is a best choice - for you. Take the time to understand your options. Talk to other women. Bring a friend to your appointment. Hormone therapy isn’t just medicine - it’s a long-term commitment to your body. Make sure it’s the right one.
Man, I read this whole thing while sipping chai at 3 AM in Delhi, and honestly? This is the clearest breakdown I’ve ever seen. Tamoxifen vs AIs isn’t just medical jargon - it’s a daily dance with your own body. I’ve got an aunt on tamoxifen - she says the hot flashes feel like living inside a tandoor, but she’d rather roast than break a hip. And the part about CYP2D6? Mind blown. In India, we don’t even test for that. Should be standard.
Let’s cut the fluff - if you’re postmenopausal and you’re not on an AI, you’re leaving survival on the table. The data is not close. 30% lower recurrence. 2.1% fewer deaths. That’s not a ‘maybe’ - that’s a mandate. If your doctor is still pushing tamoxifen for you because ‘it’s cheaper’ or ‘you’re scared of joint pain’ - find a new doctor. Your life isn’t a cost-benefit spreadsheet.
I’m two years into letrozole and I can’t pick up my toddler without wincing. But I also don’t have to worry about my uterus bleeding out of nowhere like my sister did on tamoxifen. I switched after 2 years - started with tamoxifen because my doc said my bones were already thinning. Now I’m on denosumab, doing yoga, and taking calcium like it’s my job. It’s not glamorous, but I’m alive. And I still get to hug my kids. That’s the win.
For anyone reading this and feeling overwhelmed - you’re not alone. I cried for three days after my oncologist said ‘you’ll be on this for ten years.’ But then I joined a group of women on Reddit who shared their grocery lists, their pain journals, their bad wig selfies. It helped more than any pamphlet. This isn’t just medicine - it’s a community. You don’t have to power through it alone.
How ironic that we’ve reduced a complex biological phenomenon - estrogen’s role in carcinogenesis - to a binary choice between two pharmacological caricatures. Tamoxifen, the archaic gatekeeper, and the AI, the sterile architect of hormonal annihilation. We’ve forgotten that the body is not a machine to be optimized, but a symphony of interwoven systems. The real question isn’t which drug is superior - it’s whether we’ve become so obsessed with statistical survival that we’ve lost the art of living with the consequences. And don’t get me started on camizestrant - a molecular scalpel in a world still clinging to blunt instruments.
They don’t want you to know this but AIs are linked to the CDC’s silent epidemic of bone fractures in women over 65. And tamoxifen? It’s been tied to a secret FDA memo from 2018 about uterine cancer spikes. Big Pharma doesn’t want you to see the graphs. They’re hiding the data. Why do you think they pushed AIs so hard after 2005? Because they own the patents. And now they’re selling you ‘personalized medicine’ while you’re on a 10-year drug treadmill. Wake up.
There is a fundamental error in the article’s assertion that ‘tamoxifen protects bone density.’ This is only true in premenopausal women, and even then, the effect is modest and transient. In postmenopausal women, tamoxifen has no clinically significant impact on bone mineral density compared to placebo. The author conflates mechanism with outcome. Furthermore, the claim that ‘AIs cause brain fog’ is anecdotal and unsupported by double-blind, placebo-controlled trials. Precision in language matters - especially when lives are at stake.
I’m 38, premenopausal, on tamoxifen. The hot flashes are brutal, but I don’t have joint pain. I just wanted to say - thank you for writing this. I’ve been scared to talk about this because people think it’s just ‘women’s stuff.’ But this? This is survival. And I’m still here.