Floaters After Cataract Surgery: What’s Normal and What’s Not
After cataract surgery, many people notice something unexpected: small dots, squiggles, or cobweb-like shapes drifting across their vision. It’s startling-especially when you just had surgery to see better. But here’s the truth: floaters after cataract surgery are common, and in most cases, they’re harmless. The real question isn’t whether you have them-it’s whether they’re normal or a sign of something serious.
Why You’re Seeing Floaters After Surgery
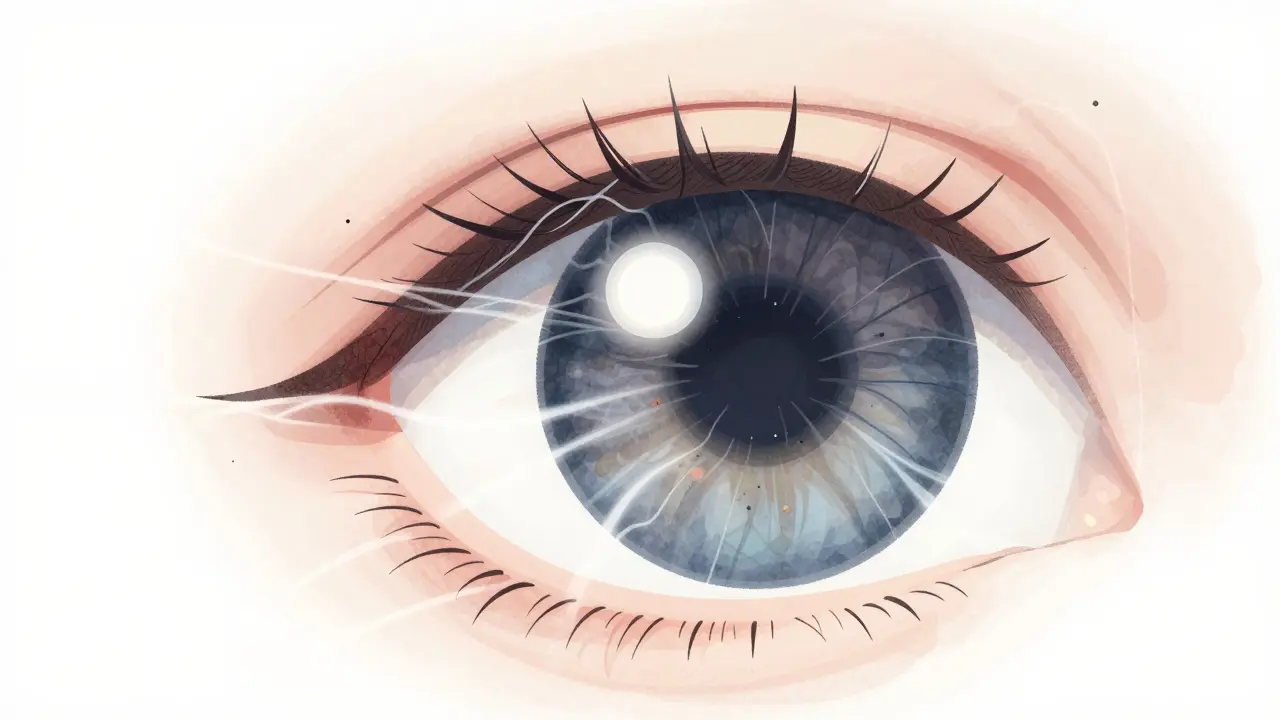
Before surgery, your vision was cloudy from the cataract. That cloudiness didn’t just blur your sight-it also hid tiny clumps of gel inside your eye called vitreous floaters. These aren’t new. They’ve been there for years, maybe decades. But now, after your cataract is removed and replaced with a clear artificial lens, everything looks sharper. And suddenly, those old floaters? They’re impossible to ignore. The vitreous is the jelly-like substance that fills the back of your eye. As you age, it slowly shrinks and pulls away from the retina. This is called posterior vitreous detachment (PVD). Cataract surgery speeds this process up. Studies show that about 28% more patients experience PVD after phacoemulsification surgery than would naturally with aging. That’s why so many people notice floaters within 24 to 48 hours after surgery. These floaters aren’t particles floating in your eye-they’re shadows cast by clumped collagen fibers inside the vitreous. When light hits them, they block a little bit of it, creating dark shapes that move when your eye moves. They’re most visible against bright backgrounds-like a white wall or a clear sky-because there’s nothing else for your eye to focus on.How Long Do They Last?
Most people don’t have to live with floaters forever. In fact, 85% of patients see a big improvement within 3 to 6 months. By 12 weeks, nearly 9 out of 10 patients either barely notice them or have completely adjusted. A 2023 survey of 1,250 patients at Diamond Vision found that 63% felt significant improvement by 6 weeks. Only 15-20% still have noticeable floaters after a year, and even then, most learn to ignore them. Your brain is good at filtering out visual noise. Over time, it learns to tune out those drifting shapes. You won’t stop seeing them, but you’ll stop caring. That’s the goal.Normal vs. Warning Signs: The 3-2-1 Rule
Here’s the critical part: most floaters are fine. But some aren’t. The difference can mean the difference between a minor annoyance and permanent vision loss. Normal floaters:- Appear gradually, not suddenly
- Stay about the same number or slowly decrease
- Don’t come with flashes of light
- Don’t block part of your vision
- 3 or more new floaters in one minute
- 2 or more flashes of light per minute
- 1 dark curtain or shadow moving across your vision
What Do Normal Floaters Look Like?
Normal floaters after cataract surgery are usually:- Small, dark gray or black specks
- Thin, thread-like lines
- Web-like or spiderweb patterns
- Moving with your eye, with a slight delay
When to Get Checked
Your surgeon will schedule follow-ups: usually at 1 week, 1 month, and 3 months. Don’t skip them. These visits aren’t just about checking your vision-they’re about checking your retina. But you don’t have to wait for your appointment if something feels wrong. If you notice any of these, call your eye doctor the same day:- Sudden increase in floaters (more than 10 new ones in a day)
- Flashes of light that feel like camera strobes
- A dark shadow creeping in from the side or top of your vision
- Sudden blurriness that doesn’t go away
Can You Treat Floaters?
If floaters stick around and really bother you, there are options-but they’re not first-line treatments. For mild cases, doctors often recommend simple tricks:- Move your eyes in slow circles to shift floaters out of your central vision
- Look up and down or side to side to let them drift away
- Use bright lighting to reduce contrast (dim rooms make floaters more obvious)
- Laser vitreolysis: A laser breaks up large floaters. Works in about 65% of cases. Low risk, but not always effective.
- Pars plana vitrectomy: Surgery to remove the vitreous gel. Success rate is 90%, but carries a 1.5% risk of complications like retinal detachment or cataract progression.
What’s New in Treatment?
Research is moving fast. A 2023 meta-analysis found that femtosecond laser-assisted cataract surgery reduces PVD-related floaters by 18% compared to traditional methods. That’s a big win for future patients. There’s also an FDA Phase III trial (NCT04567890) testing a new enzyme-based treatment that dissolves floaters without surgery. Early results show 78% reduction in floater size at 6 months-with almost no side effects. If approved, this could be a game-changer.The Bottom Line
Floaters after cataract surgery are normal. They’re not a sign your surgery failed. They’re a side effect of clearer vision revealing what was always there. But clarity also means you can’t ignore warning signs anymore. Learn the 3-2-1 Rule. Know what’s typical. And don’t wait if something feels off. Most floaters fade. But if they’re a symptom of something dangerous, timing saves your sight.Frequently Asked Questions
Are floaters after cataract surgery normal?
Yes, floaters are very common after cataract surgery. About 70% of patients notice them in the first few weeks. They’re usually pre-existing vitreous clumps that become visible after the cloudy cataract is removed. Most fade or become less noticeable within 3 to 12 weeks.
How long do floaters last after cataract surgery?
For most people, floaters improve within 3 to 6 months. By 12 weeks, 89% of patients report significant improvement or full adaptation. Only 15-20% still have noticeable floaters after a year, and even then, many learn to ignore them as their brain filters them out.
When should I worry about floaters after cataract surgery?
Worry if you suddenly see more than 3 new floaters in one minute, experience 2 or more flashes of light per minute, or notice a dark curtain or shadow in your vision. These are signs of a possible retinal tear or detachment, which require emergency care within 72 hours to prevent permanent vision loss.
Can floaters be removed without surgery?
Yes, a procedure called laser vitreolysis can break up large floaters without cutting into the eye. It’s effective in about 65% of cases and has minimal risks. But it’s not always successful, and most doctors recommend it only if floaters severely impact daily life after 6 months of trying to adapt.
Do floaters mean I need another surgery?
No, floaters alone don’t mean you need another surgery. They’re usually just a side effect of improved vision revealing old vitreous changes. Only if you develop a retinal tear or detachment-rarely triggered by floaters-would you need emergency surgery. Most patients never need further procedures.
Can I prevent floaters after cataract surgery?
You can’t fully prevent them, but newer surgical techniques like femtosecond laser-assisted cataract surgery reduce the risk of posterior vitreous detachment by 18% compared to traditional methods. Pre-op OCT scans also help identify high-risk patients. Still, floaters remain common even with the best techniques.
After cataract surgery, I noticed floaters within hours-scary at first, but the 3-2-1 Rule saved me. I tracked mine daily and realized they were stabilizing. No flashes, no shadows. Just slow fading. By week 6, I barely noticed them. Trust the process. Your brain is rewiring your visual filter, not failing you.
I was terrified when I saw those spiderweb shapes after my surgery. My surgeon said it was normal, but I didn’t believe him until I read this. Thank you for explaining why it happens-it’s not a complication, it’s just clarity revealing what was always there. I’m 8 weeks in and already feeling like I’m tuning out the noise. You’re right: the brain adapts.
As a retired ophthalmic technician, I’ve seen this a thousand times. Patients panic because they think their new lens is defective. It’s not. The vitreous has been aging for decades. The surgery just removed the fog. Floaters are the ghost of your old vision. Most settle in 3–6 months. If you’re not seeing flashes or curtains, you’re fine. And yes-eye circles help. I taught my patients to move their gaze in slow figure-eights. Works every time.
As someone who has lived with posterior vitreous detachment for over a decade, I can say with profound empathy that this article is not merely informative-it is a lifeline. The clinical precision with which it outlines the 3-2-1 Rule is nothing short of heroic in a world where medical information is often diluted into misinformation. To those trembling before the flicker of a shadow-know this: you are not alone, and your vigilance is your strength.
Let’s be honest-this is the kind of content that should be mandatory reading before cataract surgery. Most patients are given a one-page pamphlet and told to ‘call if something’s wrong.’ This? This is the difference between a patient who survives and one who loses vision. The 3-2-1 Rule isn’t just a guideline-it’s a diagnostic protocol disguised as common sense. Shame on clinics that don’t embed this in their pre-op packets.
OK, but let’s be real-this whole floaters thing is just the medical industry milking fear for profit. 😤 I had floaters after surgery, didn’t panic, and guess what? They faded. Now they’re putting out studies like this to scare people into getting unnecessary laser treatments. Laser vitreolysis? 65% success? That’s not a cure-it’s a gamble. And vitrectomy? 1.5% risk? That’s 1 in 67 people going blind from the fix. I’m not paying $3k to remove shadows I’ve lived with since 1998. 🇺🇸
While I appreciate the clinical detail, I must point out that the term 'vitreous floaters' is anatomically imprecise. The vitreous humor is a gel, not a liquid, and the collagen fibers are not 'clumps'-they are aggregates of type II collagen fibrils that have undergone syneresis. Furthermore, the reference to 'posterior vitreous detachment' as a consequence of phacoemulsification lacks nuance; the mechanical disturbance of the anterior vitreous face during capsulorhexis is the primary driver, not the removal of the lens per se. The 3-2-1 Rule is useful, but oversimplified for clinical application.
Everyone’s acting like this is some groundbreaking revelation. I had cataract surgery in 2015. Floaters? Yeah. Flashes? Nope. Did I call my doctor? No. Did I go blind? No. People these days turn every little visual quirk into a medical emergency. You’re not going to lose your vision because you see a wiggly line. Chill out. The real risk is anxiety.
Just wanted to say thank you for writing this. I’m 52 and had surgery two months ago. I was crying every night because I thought I’d ruined my vision. This article didn’t just explain what was happening-it gave me peace. I started doing the eye circles like they suggested, and now I can read without obsessing over the shadows. You’re helping people feel less alone. That matters more than you know.
There’s a quiet philosophy here: vision isn’t about perfect clarity-it’s about acceptance. The eye doesn’t show you truth. It shows you what your brain lets you see. Cataract surgery didn’t fix my sight-it revealed the imperfections I’d spent decades ignoring. The floaters? They’re not flaws. They’re reminders that I’m still human. And maybe that’s okay.
I’m a nurse who works in retina clinics. I’ve seen too many patients come in too late. One woman waited 14 days after her first flash. By then, the detachment was total. She lost 70% of her peripheral vision. This article is the reason I hand out printed copies to every post-op patient. Don’t wait. Don’t assume. If your vision changes suddenly-it’s not ‘just floaters.’ It’s a code red. And you owe it to your future self to act.
From a retinal imaging perspective, the 18% reduction in PVD incidence with femtosecond-assisted cataract surgery is statistically significant (p<0.01) and clinically relevant, particularly in high-risk cohorts with pre-existing lattice degeneration or myopia. However, the current FDA Phase III trial (NCT04567890) for enzymatic vitreolysis remains promising but lacks long-term safety data beyond 12 months. Caution is warranted before adopting as standard of care.
I saw one floater. Just one. And I freaked out. Called my doctor at midnight. They laughed. Said it was normal. I still don’t believe them.