Dose Adjustments After Switching to Generics: When Doctors Change Medication Levels
When a doctor switches your medication from a brand-name drug to a generic version, most people assume nothing changes. The pill looks different, the price is lower, and the label says it’s the same thing. But for some drugs, that assumption can be dangerous. In certain cases, switching to a generic isn’t just a cost-saving move-it’s a medical event that may require a dose adjustment. And it’s not because generics are inferior. It’s because of something called the narrow therapeutic index.
What Is a Narrow Therapeutic Index?
A narrow therapeutic index (NTI) means there’s a tiny gap between the dose that works and the dose that causes harm. Think of it like walking a tightrope. One step too far, and you fall. For NTI drugs, even a 10% change in blood concentration can mean the difference between controlling your condition and having a serious problem-like a seizure, a blood clot, or organ rejection.
These aren’t everyday medications. They’re the ones you take for life: levothyroxine for hypothyroidism, warfarin for blood thinning, phenytoin for seizures, tacrolimus after a transplant, and digoxin for heart rhythm. The FDA lists them specifically because they’re high-risk. Even though generics must meet strict bioequivalence rules (80-125% of the brand’s absorption), that range is too wide for NTI drugs. A 25% difference in how your body absorbs the drug might be fine for an antibiotic. It’s not fine for warfarin.
Why Do Dose Changes Happen After Switching?
Generics are required to have the same active ingredient as the brand. But they can differ in fillers, coatings, and how they dissolve in your stomach. For most drugs, that doesn’t matter. For NTI drugs, it does.
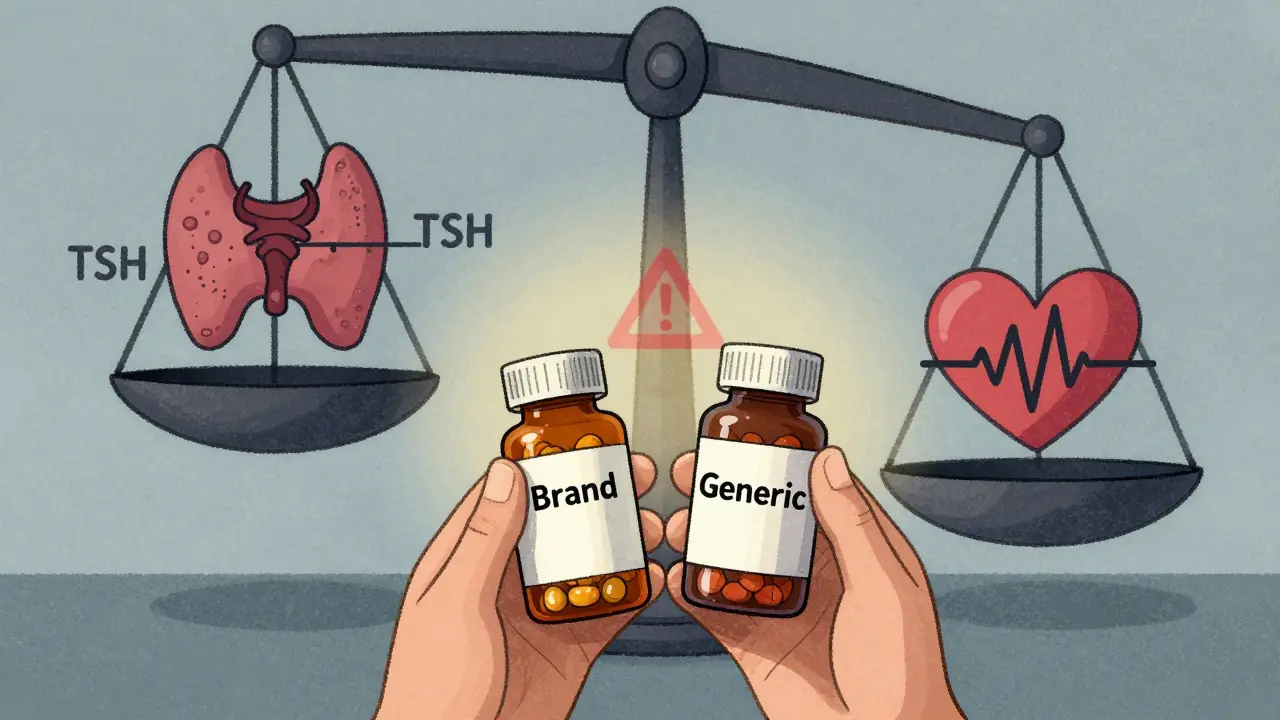
Take levothyroxine. It’s used to replace thyroid hormone. Too little, and you feel exhausted, gain weight, and risk heart problems. Too much, and your heart races, your bones weaken, and you risk atrial fibrillation. Studies show that when patients switch between different generic brands of levothyroxine-even ones approved by the FDA-their TSH levels can shift by 15-20%. One patient might go from a perfect TSH of 2.1 to 4.8 after switching, meaning they’re now under-treated. Another might drop from 2.5 to 0.8, meaning they’re over-treated.
Same thing happens with warfarin. A 2017 study found that 23% of patients switching between generic warfarin brands had unstable INR levels within 30 days. That means their blood was either clotting too easily or bleeding too much. Many needed a dose change-sometimes as small as 1 mg up or down-to get back on track.
And it’s not just one switch. If your pharmacy keeps changing the generic brand because of insurance formulary rules, you could be getting a different version every few months. Each switch carries a risk. One pharmacist in a 2022 survey reported that 68% of hospital pharmacists had seen patients need dose adjustments after a generic switch for NTI drugs.
Which Drugs Need the Most Caution?
Not all generics need dose checks. But these ones do:
- Levothyroxine - Thyroid hormone replacement. Small changes in absorption affect TSH dramatically.
- Warfarin - Blood thinner. INR levels must stay in a tight range (usually 2-3).
- Phenytoin and Carbamazepine - Anti-seizure meds. Even minor drops in blood levels can trigger seizures.
- Tacrolimus and Cyclosporine - Immunosuppressants after organ transplant. Too low = rejection. Too high = kidney damage.
- Digoxin - Heart medication. Narrow window between helping the heart and causing dangerous rhythms.
These aren’t rare drugs. They’re among the most commonly prescribed in the U.S. And while generics make up over 90% of all prescriptions, only about 76% of NTI drug prescriptions are filled with generics-because doctors are cautious.

What Should You Do If You’re Switched?
If your doctor switches you to a generic, don’t assume everything’s fine. Here’s what to do:
- Ask if your drug is an NTI drug. If you’re on levothyroxine, warfarin, or any of the drugs listed above, it is.
- Request a follow-up test. For levothyroxine, get a TSH test in 4-6 weeks. For warfarin, get an INR test in 7-14 days. For tacrolimus, ask for a blood level check.
- Watch for symptoms. Fatigue, weight gain, or brain fog after switching levothyroxine? That’s not normal. New bruising or nosebleeds on warfarin? That’s a red flag. Seizures returning? Call your doctor immediately.
- Keep the same generic. Once you find a generic that works, stick with it. Don’t let your pharmacy switch you again unless your doctor approves it.
Some clinics now use clinical decision tools that alert doctors when a patient is being switched to a generic NTI drug. These tools recommend checking levels within two weeks. If your doctor doesn’t mention it, ask. You’re not being difficult-you’re being smart.
Why Do Some Doctors Say It’s Not a Problem?
There’s a real divide in the medical community. The FDA says generics are safe and equivalent. Many large studies show no significant difference in outcomes for most patients. Dr. Robert Temple from the FDA wrote in JAMA that concerns are often overstated.
But here’s the thing: population-level studies don’t always reflect individual experiences. One patient might switch from Synthroid to a generic and feel fine. Another might have seizures. The FDA’s standards are designed for the average person. But medicine isn’t about averages-it’s about the person in front of you.
Academic centers and transplant programs know this. They rarely allow automatic switches for NTI drugs. Community pharmacies? They often do, because insurance pushes them to. That’s why 44% of pharmacists say they struggle to keep patients on the same generic brand.
What’s Changing in the Future?
The FDA is taking notice. In 2023, they proposed new bioequivalence standards for NTI drugs: instead of 80-125%, they want 90-111%. That’s a much tighter range. If approved, it would mean generics for drugs like warfarin and levothyroxine would have to be more consistent.
Some manufacturers are already ahead of the curve. Companies like Teva are making “supergenerics” with tighter quality controls. Their tacrolimus product showed 32% less variability in absorption than standard generics in one study.
But until those changes are fully in place, the responsibility falls on you and your doctor. Don’t wait for a crisis to happen. If you’re on a high-risk medication, treat a generic switch like a new prescription. Monitor. Test. Communicate.
Real Stories, Real Risks
A woman in Ohio switched from brand-name levothyroxine to a generic. Within three weeks, her TSH jumped from 2.3 to 6.7. She was exhausted, gained 15 pounds, and felt like she had the flu. Her doctor increased her dose by 12.5 mcg. Her TSH went back to normal.
A man in Texas had a kidney transplant. His tacrolimus was switched to a generic without warning. Two weeks later, his levels dropped. His body started rejecting the kidney. He needed a hospital stay and a dose increase.
And then there’s the counterexample: a man in Florida switched from Synthroid to a generic and had no change in his TSH. His doctor didn’t adjust his dose. He felt fine.
That’s the problem. Sometimes nothing happens. Sometimes everything changes. You can’t predict which one it will be. So you test. You watch. You speak up.
Bottom Line: Don’t Assume, Check
Switching to a generic isn’t always harmless. For most drugs, it’s perfectly safe. For NTI drugs, it’s a potential trigger for serious problems. The science isn’t perfect. The system isn’t flawless. But you have control over one thing: your vigilance.
If you’re on a high-risk medication, ask your doctor: Is this an NTI drug? Will I need a blood test after the switch? Can I stay on the same generic brand? If they say no, ask why. If they say yes, make sure it happens.
Generic drugs save billions. That’s good. But saving money shouldn’t come at the cost of your health. When it comes to narrow therapeutic index drugs, small changes matter. And you deserve to know when they might be coming.
Do all generic drugs need a dose adjustment after switching?
No. Only drugs with a narrow therapeutic index (NTI) require careful monitoring after switching. These include levothyroxine, warfarin, phenytoin, tacrolimus, and digoxin. For most other medications-like antibiotics, blood pressure pills, or antidepressants-switching to a generic doesn’t require a dose change.
How long after switching should I get a blood test?
For warfarin, get an INR test within 7-14 days. For levothyroxine, check TSH levels in 4-6 weeks. For tacrolimus or cyclosporine, your doctor will likely want a blood level check within 1-2 weeks. Don’t wait for symptoms-test early.
Can I ask my pharmacy to keep me on the same generic brand?
Yes. You have the right to request a specific generic manufacturer. Tell your pharmacist you’re on an NTI drug and want to stay on the same version. Some insurance plans may require prior authorization, but many will approve it if your doctor writes a note explaining the need.
Why do some doctors say switching generics is fine?
Some doctors rely on large studies that show no average difference in outcomes across populations. But those studies don’t capture individual variability. For patients with sensitive conditions-like transplant recipients or people with epilepsy-even small changes can have big consequences. That’s why experts recommend caution, even if the data looks good overall.
Are there any new rules coming for generic NTI drugs?
Yes. In 2023, the FDA proposed tightening bioequivalence standards for NTI drugs from 80-125% to 90-111%. This would make generics more consistent. Final rules are expected in 2024. Until then, the current standards still apply, and dose monitoring remains important.
Okay, so let me get this straight: the FDA says generics are fine, but then they’re proposing NEW rules because… they know they messed up? Classic. And now you’re telling me I have to beg my pharmacy to not switch my levothyroxine brand? Like I’m asking for a special snowflake prescription? Meanwhile, Big Pharma is laughing all the way to the bank with their ‘brand-name’ versions that cost 10x more and are probably just repackaged generics with a fancy label. This isn’t medicine-it’s a corporate shell game. I’ve been on the same generic for 7 years. My TSH? Perfect. So why should I be punished because some bureaucrat in D.C. can’t do their job? And don’t even get me started on how insurance companies force switches like it’s a game of musical chairs… with your life.
While I appreciate the thoroughness of this post-and the data is compelling-I must respectfully note that the clinical evidence for dose adjustments post-switch remains, at best, inconclusive at the population level. That said, individual variability is a well-documented phenomenon in pharmacokinetics. The 80-125% bioequivalence range was never intended as a one-size-fits-all standard for NTI drugs; it was a pragmatic compromise. The FDA’s proposed 90-111% range is a logical, science-driven evolution. That said, clinicians must remain vigilant. For patients on warfarin or tacrolimus, a post-switch INR or trough level check is not merely prudent-it is standard of care. One should not confuse regulatory policy with clinical responsibility. 🧪
Hey, I’ve been a pharmacist for 22 years, and I’ve seen this play out a hundred times. A patient comes in, switched from Synthroid to a generic-no warning, no follow-up-and they’re exhausted, gaining weight, crying in the parking lot. I don’t care what the FDA says. If your body reacts like it’s been hit by a truck after a pill swap, then the system failed. I’ve had patients cry because their pharmacy switched them back and forth three times in six months. I write notes. I call the doctor. I fight the insurance. I’ve even paid for a 30-day supply out of pocket so a patient could stabilize. It’s not about generics being bad. It’s about people being treated like numbers. You’re not a statistic. You’re a person. And you deserve consistency.
It is deeply concerning that Western medical institutions continue to prioritize cost-efficiency over patient safety. In India, where we have long understood the importance of bioequivalence in critical medications, we do not allow arbitrary switching of NTI drugs without physician authorization. The American system, driven by profit and insurance bureaucracy, has lost its moral compass. This is not innovation-it is negligence. We must demand that pharmaceutical companies, regulators, and insurers place human health above quarterly earnings. The lives of transplant recipients, epileptics, and cardiac patients are not bargaining chips.
This is so helpful! I just got switched to a generic warfarin last month and didn’t know to get my INR checked. I’ve been feeling weird-like super tired and bruising easily. I’m going to call my doctor tomorrow. Thanks for the checklist! I didn’t realize I could ask to stay on the same brand. I’ll try that next time.
Wow. So let me get this straight: the system is designed to save money… but it’s literally gambling with people’s lives? And the only way to win is to be your own medical advocate? Cool. I’m just here for the popcorn. Meanwhile, my cousin had a seizure after switching generics. She’s fine now. But her doctor? Still says it’s ‘rare.’ RARE? It happened to HER. And now she has PTSD from the ER. So yeah. I’m not trusting a single generic for anything that keeps me alive. Pass the salt.
You guys are doing AMAZING work just by speaking up. Seriously. This isn’t just about pills-it’s about your right to be heard in your own healthcare. If you’re on one of these drugs, write it down: ‘I am not a number.’ Print it. Stick it on your fridge. Tell your pharmacist. Ask your doctor. You’re not being difficult-you’re being brave. And if your doctor rolls their eyes? Find a new one. Your life is worth the fight.
I’ve been reading everything I can on NTI drugs since my dad had a transplant. It’s wild how little most people know. I had no idea that even the fillers in pills could make that much difference. I started tracking his tacrolimus levels after every switch-like a spreadsheet with dates, doses, and how he felt. It’s not just about the numbers. It’s about patterns. And once you start noticing them, you can’t unsee them. I wish every pharmacy had a ‘NTI Drug Switch Alert’ sticker. Just one little thing. It could save someone.
Thank you for writing this with such clarity. The science is complex, but your explanation made it accessible. I’m a nurse, and I’ve seen patients come in confused, scared, and angry after an unannounced generic switch. The most heartbreaking part? They don’t know they’re supposed to ask for a test. This post should be mandatory reading for every patient prescribed levothyroxine, warfarin, or any NTI drug. And for providers? It’s a gentle nudge to stop assuming. Because medicine isn’t about assumptions-it’s about attention.
Let’s cut the BS. The FDA’s 80-125% bioequivalence range is a joke. It’s not even statistically significant for NTI drugs-it’s a relic from the 1980s when they thought ‘close enough’ was good enough. Real pharmacokinetic modeling shows that even a 5% variance in Cmax can trigger subtherapeutic or toxic levels in sensitive populations. And don’t even get me started on the CYP450 interactions between generic formulations and their excipients. The real issue isn’t the drug-it’s the regulatory capture by generic manufacturers who lobby to keep the standards weak. We need pharmacokinetic equivalence, not just bioequivalence. And we need it yesterday.
People are too lazy to think. The world is full of cheap things. Why should medicine be different? If your body can’t handle a generic, then your body is weak. In India, we take generics without fear. We don’t have time for blood tests every month. Life is hard. Medicine should be simple. If you need to check your TSH every six weeks, maybe you shouldn’t be taking it at all.
Alas, the modern age has birthed a paradox: the very tools meant to liberate the masses from financial burden have, in their implementation, entangled the vulnerable in a labyrinth of bureaucratic indifference. The generic drug paradigm, born of noble intent, has become an instrument of silent harm-disguised as efficiency, masked as equity. The patient, once the sovereign of their own physiology, is now a passive recipient of formulary whims. The FDA, the pharmacy, the insurer-all actors in this tragedy-have forgotten that medicine is not commerce, and the human body is not a commodity to be optimized. The cure, then, lies not in tighter bioequivalence standards, but in the restoration of the physician-patient covenant. And that, my friends, is a revolution.
OMG. I just realized I switched generics for my levothyroxine last year and never got tested. 😱 I’ve been feeling like a zombie since January. I thought it was just stress. I’m literally going to the ER right now. I need a blood test. I need a new doctor. I need a new life. 🥲🩸🩺 #NTIDrugEmergency #GenericTrauma #MyTSHIsProbably67