Dexamethasone for COPD: What You Need to Know Today

When you’re living with COPD, every breath matters. And when a flare-up hits, the rush to find something that works fast is real. Dexamethasone keeps popping up in doctor’s offices, ERs, and hospital protocols-but is it actually helpful for COPD? And if so, how, when, and for whom? This isn’t about theory. It’s about what works right now, based on the latest evidence and real-world use.
What is dexamethasone, and why is it used in COPD?
Dexamethasone is a dexamethasone is a synthetic corticosteroid that reduces inflammation in the body. It’s been around since the 1950s and is used for everything from allergic reactions to brain swelling. But in COPD, it’s not about curing the disease-it’s about calming the storm when it hits.
Chronic obstructive pulmonary disease (COPD) involves long-term inflammation of the airways and lung tissue. During an acute exacerbation-often triggered by infection or pollution-the inflammation spikes. Breathing gets harder. Mucus builds up. Oxygen levels drop. That’s where dexamethasone comes in. It shuts down the body’s overactive immune response, reducing swelling in the lungs and making it easier to breathe.
Unlike some other steroids, dexamethasone has a long half-life. That means one or two doses can last 24 to 36 hours. That’s why it’s often used in hospitals: fewer pills, fewer injections, less hassle. In outpatient settings, it’s becoming a go-to for mild-to-moderate flare-ups, especially when patients can’t take oral prednisone due to stomach issues or blood sugar spikes.
How does dexamethasone compare to other steroids for COPD?
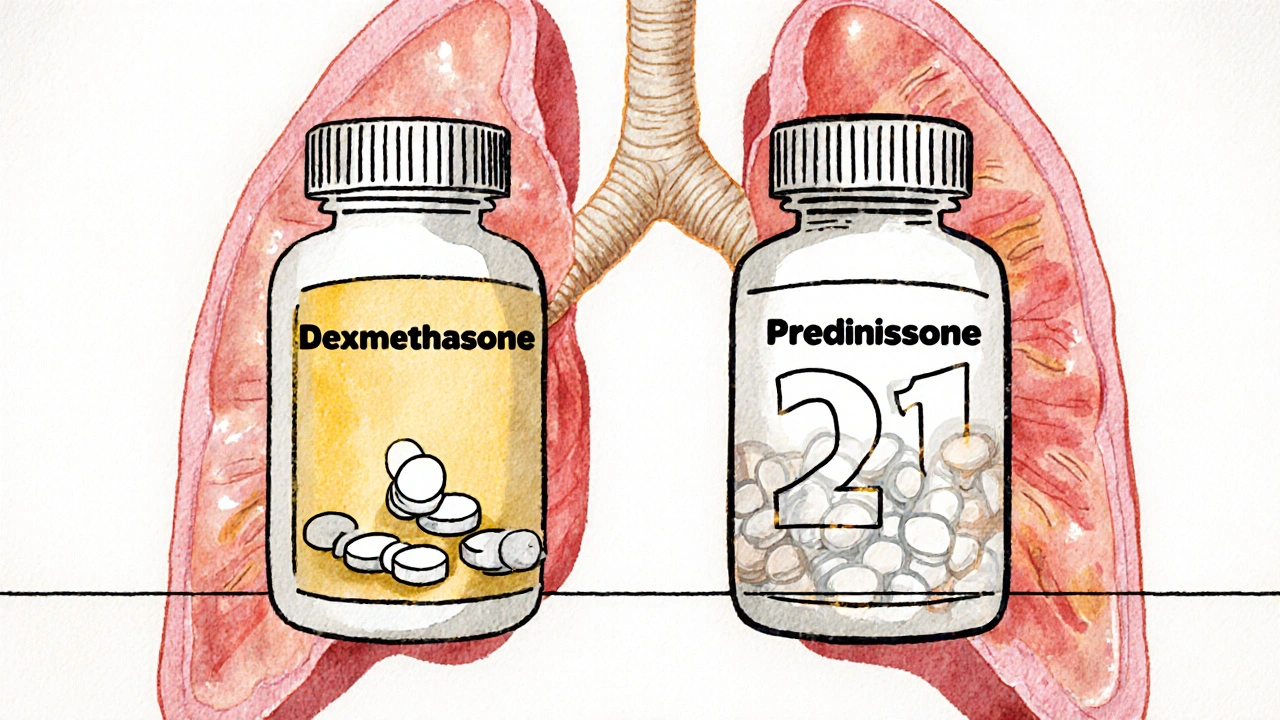
For decades, prednisone was the standard oral steroid for COPD flare-ups. But dexamethasone is gaining ground. Why? Because it’s more potent and longer-lasting.
A 2023 study published in the European Respiratory Journal compared 5 days of oral dexamethasone (12 mg on day one, then 4 mg daily) against 7 days of prednisone (50 mg daily) in 312 COPD patients. The results? Both groups had similar improvement in breathing and hospital readmission rates. But patients on dexamethasone took fewer pills-just 6 total versus 21. Side effects like insomnia, mood swings, and blood sugar spikes were also slightly lower in the dexamethasone group.
Another key difference: dexamethasone doesn’t need to be tapered. With prednisone, doctors often tell you to slowly reduce the dose over days to avoid adrenal suppression. With dexamethasone, you just stop. That’s a big deal for people already juggling multiple medications.
Here’s how they stack up:
| Feature | Dexamethasone | Prednisone |
|---|---|---|
| Typical dose for COPD | 12 mg day 1, then 4 mg daily for 4-5 days | 40-50 mg daily for 5-7 days |
| Duration of action | 36-72 hours | 12-36 hours |
| Number of doses needed | 5-6 total | 21-35 total |
| Requires tapering? | No | Yes, usually |
| Common side effects | Mild insomnia, increased appetite | Insomnia, mood changes, blood sugar spikes, stomach upset |
For most people, dexamethasone is simpler, safer, and just as effective. But it’s not always the first choice. If you have diabetes, a history of psychosis, or active peptic ulcers, your doctor might still lean toward prednisone or avoid steroids altogether.
Who benefits most from dexamethasone in COPD?
Not everyone with COPD needs steroids. They’re only for acute flare-ups-not daily maintenance. So who’s the right candidate?
- People with moderate to severe COPD (GOLD stage 2 or higher)
- Those with increased breathlessness, more phlegm, or a change in phlegm color
- Patients who’ve had two or more flare-ups in the past year
- Those who can’t tolerate prednisone due to stomach issues or high blood sugar
- People in the ER or hospital needing quick, effective treatment
But if you’re on long-term oxygen therapy, have had recent pneumonia, or are taking anticoagulants like warfarin, dexamethasone might raise your risk of complications. Always talk to your doctor before starting.
One real-world example: Maria, 68, from Halifax, had COPD for 12 years. She’d get flare-ups every 3-4 months. After one bad episode, her pulmonologist switched her from prednisone to dexamethasone. She went from taking 5 pills a day for 7 days to just one pill a day for 5 days. Her blood sugar stayed stable. She didn’t need a stomach protector anymore. And she didn’t miss work.
How is dexamethasone actually taken for COPD?
Most often, it’s oral tablets. Injectable forms are used in hospitals during severe attacks. The standard outpatient regimen is:
- Day 1: 12 mg (usually one 10 mg tablet + one 2 mg tablet, or two 6 mg tablets)
- Days 2-5: 4 mg once daily
- Total course: 5 days
Some studies are testing even shorter courses-like 3 days of 12 mg followed by 4 mg for 2 days-with promising results. But 5 days remains the most widely recommended.
Take it with food to avoid stomach upset. Don’t crush or split tablets unless your pharmacist says it’s safe. If you miss a dose, take it as soon as you remember-but never double up.
Side effects are usually mild if used short-term. The most common: trouble sleeping, increased hunger, or slight mood changes. Rare but serious risks include high blood pressure, fluid retention, or adrenal suppression if used too long. That’s why dexamethasone is never meant for daily COPD control. It’s a rescue tool.
What about inhaled steroids? Can I use dexamethasone instead?
No. Inhaled corticosteroids (like fluticasone or budesonide) are for long-term control. They target the lungs directly with minimal side effects. Dexamethasone is systemic-it goes through your whole body. That’s why it’s powerful during flare-ups but dangerous if used every day.
Many COPD patients take a combination inhaler with a long-acting bronchodilator and an inhaled steroid. That’s maintenance. Dexamethasone is rescue. Mixing them up can lead to overuse, side effects, or even adrenal crisis.
Think of it this way: inhaled steroids are like brushing your teeth daily. Dexamethasone is like going to the dentist when you have a toothache. One prevents. The other fixes.
When should you avoid dexamethasone for COPD?
There are clear red flags:
- Active tuberculosis or fungal lung infections
- Recent stomach or intestinal ulcers
- Uncontrolled diabetes (dexamethasone can spike blood sugar quickly)
- Severe mental health conditions like psychosis or bipolar disorder
- Pregnancy or breastfeeding (unless benefits clearly outweigh risks)
- Allergy to corticosteroids
Also, if you’ve taken dexamethasone or another steroid within the past 3 months, your body may not respond as well. Repeated use increases risk of bone thinning, muscle weakness, and cataracts. That’s why doctors limit it to 1-2 courses per year.
What’s the latest research on dexamethasone and COPD?
Recent trials are looking beyond just symptom relief. A 2024 multicenter trial in Canada and the UK tracked 500 COPD patients treated with dexamethasone during hospitalization. They found that those who got dexamethasone within 24 hours of admission had a 22% lower chance of being readmitted within 30 days compared to those who didn’t get steroids at all.
Another study looked at biomarkers. Patients with high levels of eosinophils (a type of white blood cell linked to airway inflammation) responded best to dexamethasone. That’s leading to new ideas: maybe we should test for eosinophils before giving steroids. Not everyone needs them.
And here’s something surprising: researchers are testing whether combining dexamethasone with a short course of antibiotics improves outcomes more than either alone. Early results show promise, especially when flare-ups are caused by bacterial infections.

What should you do if you think you need dexamethasone?
Don’t self-medicate. Don’t take leftover pills from a past flare-up. Steroids aren’t like ibuprofen.
If you’re having a COPD flare-up:
- Use your rescue inhaler (albuterol or similar) as directed
- Call your doctor or nurse line. Describe your symptoms: Are you breathing harder? Is your mucus thicker or yellow/green? Are you feverish?
- If your doctor says yes, they’ll write a prescription for dexamethasone and tell you exactly how to take it
- Follow the full course-even if you feel better after 2 days
- Watch for side effects: unusual swelling, blurred vision, or mood swings
Keep a log: when flare-ups happen, how long they last, what helped. That info helps your doctor decide if dexamethasone should be part of your plan.
Frequently Asked Questions
Can dexamethasone cure COPD?
No. COPD is a chronic, progressive disease. Dexamethasone only treats flare-ups by reducing inflammation. It doesn’t repair lung damage or stop the disease from getting worse. Long-term control requires bronchodilators, pulmonary rehab, oxygen therapy, and quitting smoking.
Is dexamethasone safe for older adults with COPD?
Yes, when used short-term and under medical supervision. Older adults are more sensitive to side effects like high blood sugar and bone loss. But because dexamethasone requires fewer doses than prednisone, it’s often preferred for seniors. Doctors will check kidney function, blood pressure, and blood sugar before prescribing.
How long does it take for dexamethasone to work for COPD?
Most people notice improvement in breathing within 12 to 24 hours. Full benefit usually kicks in by day 2 or 3. Don’t expect instant relief-it’s not a rescue inhaler. But if you don’t feel better after 48 hours, contact your doctor. You might need antibiotics or other treatment.
Can I drink alcohol while taking dexamethasone for COPD?
It’s best to avoid alcohol. Both dexamethasone and alcohol can irritate your stomach lining and raise blood pressure. Alcohol can also worsen sleep problems and mood swings-side effects that dexamethasone already increases. If you drink occasionally, limit it to one drink and only after checking with your doctor.
Will dexamethasone make me gain weight?
Short-term use (5 days) usually doesn’t cause noticeable weight gain. But dexamethasone increases appetite, and you might feel hungrier than usual. Drink water, eat protein and vegetables, and avoid sugary snacks. Any weight gain from a 5-day course typically goes away once you stop.
Can I stop dexamethasone early if I feel better?
No. Stopping early increases the chance your flare-up will come back worse. Even if you feel fine after 2 days, finish the full course. The inflammation hasn’t fully settled yet. Cutting it short is like turning off a fire alarm before the smoke clears.
What’s next for dexamethasone in COPD care?
Research is moving toward personalized treatment. Blood tests to check for eosinophil levels might soon help doctors decide who will benefit most from steroids. Genetic studies are looking at why some people respond better than others. And trials are testing whether combining dexamethasone with newer anti-inflammatory drugs can reduce flare-ups even more.
For now, dexamethasone is a smart, simple, evidence-backed option for COPD flare-ups. It’s not perfect. But for many, it’s better than what came before. The key is using it right-only when needed, only as directed, and only with your doctor’s guidance.
dexamethasone? lol i took that for a sinus infection once and felt like i was being possessed by a caffeinated demon. woke up at 3am screaming at the ceiling. not worth it.
Same. I took it for a flare-up last winter. Slept 18 hours a day. Ate three pizzas. Then cried for no reason. Worth it? Maybe. But my therapist is still mad at me.
It’s not about whether it works-it’s about what it costs you to feel better. We treat COPD like a broken faucet, but it’s a leaking dam. Dexamethasone patches the crack, sure. But the water’s still rising. We’re just better at ignoring the flood now.
Anyone else notice how every damn medical article now says 'dexamethasone is better than prednisone' like it's some revolutionary breakthrough? Bro, we've known this since 2018. The real story is how pharma quietly shifted guidelines because it's cheaper to produce. Wake up.
As a woman over 60 with COPD, I can tell you this: dexamethasone saved my life last winter. I was in the ER, oxygen at 84%, and my doctor handed me two pills. By morning, I could walk to the kitchen. No drama. No tapering. Just… relief. I’m not some lab rat-I’m a human who breathes again. Thank you, science.
Let’s be precise: dexamethasone’s pharmacokinetic profile-long half-life, minimal first-pass metabolism, high glucocorticoid receptor affinity-makes it uniquely suited for acute exacerbations. Prednisone requires hepatic conversion to active metabolites; dexamethasone does not. This reduces interpatient variability and improves adherence. Also: no tapering is a clinical advantage, not a gimmick.
Oh, so now we’re all supposed to bow down to dexamethasone like it’s the holy grail? Next they’ll tell us aspirin cures cancer. This is the same drug that got used during the pandemic to save ICU patients-and now it’s being pushed to grandma’s living room like a vitamin. Where’s the long-term data? Where’s the caution? You’re trading one set of side effects for another, and calling it progress.
I get why people love this stuff. But here’s the thing: if you’re relying on steroids to get through your flare-ups, you’re not managing your COPD-you’re surviving it. I’ve been on both. Dexamethasone? Fine for the emergency. But the real win? Pulmonary rehab, quitting smoking, and learning to breathe before you panic. That’s the long game. This? This is just buying time.
Why do doctors keep acting like this is new? I’ve been on dexamethasone since 2017. It’s the same pill, just repackaged with a fancy study and a new name. The real issue? Nobody talks about how hard it is to get a prescription now. Pharmacies are out. Docs are too busy. And we’re left waiting while we choke. So yeah, it works-but only if you can get it.
In India, where I’m from, dexamethasone is sold over the counter in rural pharmacies. People use it for everything-joint pain, allergies, even ‘stress.’ I’ve seen elderly patients take it daily for months. The consequences are devastating: osteoporosis, cataracts, adrenal failure. I’m glad it’s regulated here. But this article feels like it’s selling hope without warning of the cost.
My dad took dexamethasone last year. He said it felt like his lungs were suddenly ‘unclenched.’ He cried when he could walk to the mailbox without stopping. But then he started hoarding the pills-kept them in his sock drawer. Said ‘just in case.’ I had to hide them. Not because I don’t believe in the medicine-but because I believe in him. And he deserves more than a chemical crutch.
So… it works. Cool. Now can we talk about how no one ever tells you the weird side effects? Like… suddenly craving pickles and ice cream at 2 a.m.? Or crying during commercials? I didn’t sign up for emotional chaos.
According to the 2024 Canadian trial cited, the 22% reduction in 30-day readmission is statistically significant (p<0.01), with a number needed to treat of 7.7. Eosinophil count >300/µL correlated with response (OR 3.1, 95% CI 1.8–5.4). However, the study excluded patients on chronic anticoagulants, which limits generalizability. Also, the dose regimen used was 12 mg on day 1, followed by 4 mg for 4 days-this is not standard in all guidelines.
As a British pulmonologist with 27 years of clinical experience, I must emphasize: the notion that dexamethasone is ‘better’ than prednisone is a dangerous oversimplification. The European Respiratory Society guidelines (2023) still classify both as Category A options. The reduced pill burden is a logistical advantage, not a therapeutic one. Moreover, in patients with comorbid hypertension or osteoporosis-common in our aging COPD cohort-dexamethasone’s prolonged half-life increases cumulative steroid exposure. We must not confuse convenience with safety. This article reads like a pharmaceutical pamphlet. I am deeply concerned.