Corticosteroid Injections for Joint Pain: What They Do, How Long They Last, and When to Avoid Them

When your knee, shoulder, or hip starts hurting like it’s been hit by a truck - and over-the-counter painkillers don’t touch it - your doctor might suggest a corticosteroid injection. It’s one of the most common treatments for joint pain, especially when swelling and stiffness are the main problems. But what exactly does it do? Does it fix the problem, or just hide it? And how many times can you get one before it starts doing more harm than good?
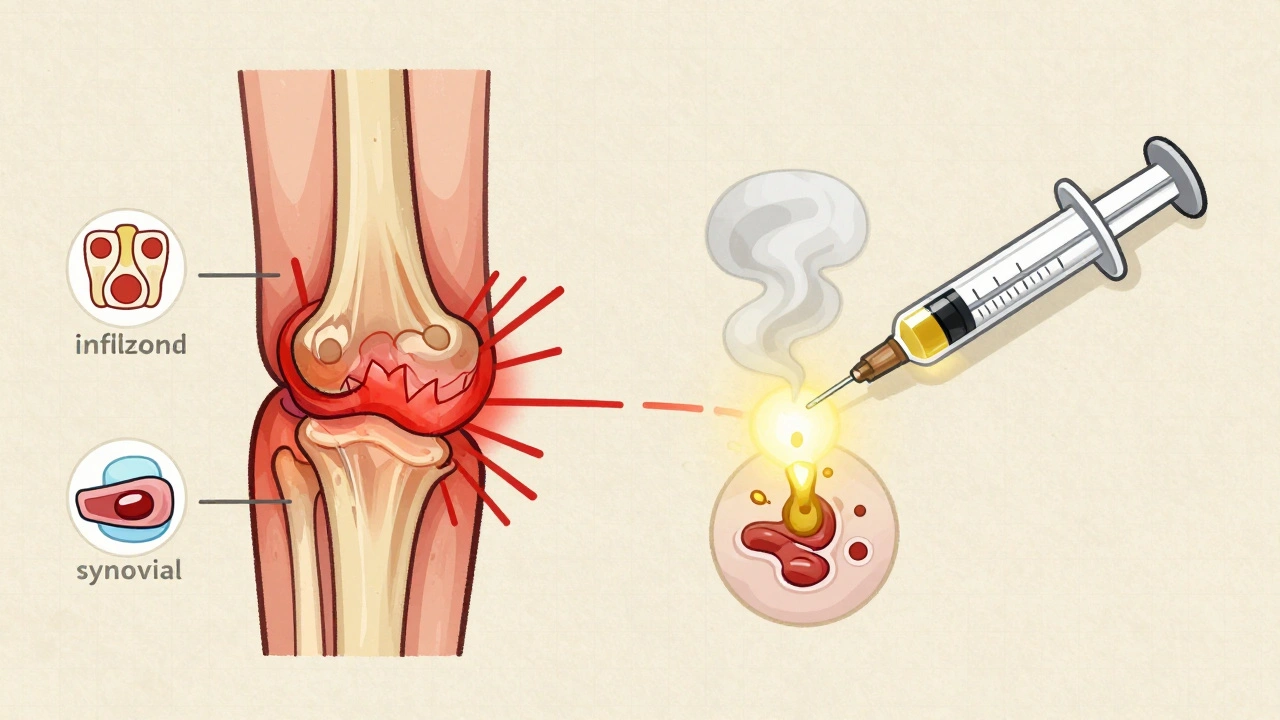
How Corticosteroid Injections Actually Work
Corticosteroid injections, often called cortisone shots, aren’t painkillers. They don’t numb your nerves like lidocaine does. Instead, they fight inflammation at the source. Inside your joint, inflamed tissue releases chemicals that make nerves scream. Corticosteroids shut down that signal. They enter the cells lining your joint and turn off genes that produce inflammatory proteins like interleukin-1 and tumor necrosis factor-alpha. This reduces swelling, heat, and tenderness. The result? Less pressure on nerves, less pain. These injections usually mix a slow-release corticosteroid - like triamcinolone acetonide or methylprednisolone acetate - with a fast-acting numbing agent like lidocaine. You feel the numbing effect right away, but the real magic takes 24 to 72 hours. That’s when the anti-inflammatory action kicks in. The dose depends on the joint. A big joint like the knee might get 40 to 80 milligrams. A small joint like the wrist or finger? Maybe 10 to 20 milligrams. The goal isn’t to flood the area - it’s to calm it down just enough.How Long Does the Relief Last?
This is where expectations matter. Most people feel better within a few days. For some, the relief lasts 3 to 6 weeks. For others, it’s 8 to 12 weeks. But here’s the hard truth: corticosteroid injections don’t cure anything. They don’t repair torn cartilage, fix worn-out tendons, or reverse osteoarthritis. They just put a pause on the inflammation. A 2023 meta-analysis of 15 studies found that corticosteroid injections gave modest pain relief compared to saline placebo - but only for the first 2 to 4 weeks. After 6 weeks, there was no difference. At 24 weeks? No benefit at all. That’s why doctors don’t recommend them for long-term management of chronic joint degeneration. Some people get lucky. One patient from the Arthritis Foundation community reported returning to competitive golf just 10 days after a hip bursitis injection and stayed pain-free for 12 weeks. But others aren’t so lucky. Reddit users frequently report diminishing returns: the first shot lasts 8 weeks, the second only 5, the third barely 3. And sometimes, the injection itself triggers a flare-up - a painful, temporary worsening that can last 2 to 3 days. About 34% of dissatisfied patients cite this as their main complaint.Who Benefits Most?
Corticosteroid injections shine in acute, inflammatory conditions:- Acute gout flares - They reduce swelling faster than oral meds.
- Bursitis - Especially in the shoulder or hip.
- Tendinitis - Like tennis elbow or rotator cuff inflammation.
- Rheumatoid arthritis flares - When multiple joints are inflamed.
The Risks: What No One Tells You
The biggest fear? That repeated shots damage your joint. And it’s real. Corticosteroids suppress collagen production - the very protein that holds tendons and cartilage together. Over time, this can weaken tissues. A 2023 study found patients who got repeated knee injections had over 3 times higher odds of radiographic joint damage worsening. Those who got them frequently? Nearly 5 times higher risk. Other risks include:- Tendon rupture - Especially in the Achilles or rotator cuff. This is rare, but more likely if you’ve had multiple injections or keep using the joint too soon.
- Joint infection - Extremely rare (less than 1 in 1,000), but the risk spikes if you’ve had an injection within 3 months before joint replacement surgery. One study found these patients were more than twice as likely to get a prosthetic joint infection.
- Skin changes - Lightening or thinning of the skin at the injection site. More common with repeated use in visible areas like the face or hands.
- Blood sugar spikes - Diabetics need to monitor glucose for 72 hours after the shot. A temporary rise is normal, but it can be dangerous if unmanaged.
How Often Is Too Often?
There’s no universal rule, but experts agree on limits. The American College of Rheumatology recommends no more than 3 to 4 injections per joint per year. Many doctors stick to 2 or 3. If you’re getting one every 6 weeks for 6 months straight, you’re pushing the edge. Dr. Benjamin Domb of the American Hip Institute says injections are safe every three months - as long as you’re not seeing worsening pain or structural damage on imaging. But if your pain returns faster than 8 weeks, it’s a sign the problem isn’t just inflammation. It’s structural. And that’s when you need a different plan: physical therapy, bracing, or even surgery.Ultrasound Guidance: Why It Matters
A shot given “blind” - without imaging - misses the joint nearly 30% of the time. That means you’re getting a needle in the wrong spot, wasting money, and getting no relief. Ultrasound guidance increases accuracy from 70% to 95%. It’s not always available, but if you’re getting a shot in a small or deep joint - like the wrist, ankle, or hip - ask for it. It’s worth the extra cost.Cost and Alternatives
Without insurance, a corticosteroid injection costs $100 to $300. Compare that to PRP (platelet-rich plasma) therapy, which runs $500 to $1,500, or viscosupplementation (hyaluronic acid), which costs $500 to $1,000. Corticosteroids win on price and speed. But alternatives are rising. PRP and stem cell therapies show promise for longer-term healing, especially in early osteoarthritis. However, they don’t work as fast. If you need to get back on your feet in 48 hours - for a job, a game, or just to sleep - corticosteroids still win. A new FDA-approved option, Zilretta (extended-release triamcinolone), offers relief for up to 12 weeks in about 45% of osteoarthritis patients. That’s better than standard shots, but still not a cure.What to Do After the Shot
Don’t treat it like a magic fix. After the injection:- Avoid heavy lifting or strenuous activity for 48 hours. You’re in a temporary window of reduced pain - but your joint is still healing. Overuse can trigger a flare or injury.
- Use ice if you feel warmth or swelling. A post-injection flare is common and usually fades in 2 to 3 days.
- Keep moving gently. Light walking or range-of-motion exercises help prevent stiffness.
- If you’re diabetic, check your blood sugar twice daily for 3 days.
- Track your pain. Use a simple scale: 0 (no pain) to 10 (worst pain). Note when it peaks and when it drops. That helps your doctor decide if another shot makes sense.
When to Say No
You should avoid corticosteroid injections if:- You have an active infection anywhere in your body.
- You’re allergic to corticosteroids or local anesthetics.
- You’ve had a joint replacement in the past 3 months.
- Your joint shows advanced bone-on-bone wear on X-ray - and you’ve already had 2 or more injections this year.
- Your pain isn’t improving after 2 injections, even with ultrasound guidance.
life is pain bro 🤷♂️ injections just delay the inevitable
i got one in my knee last year and it felt like a hot needle full of rage was injected into my soul. then it worked for 6 weeks. then my dog started limping and i realized i was the one who broke my own body by ignoring the real problem. lol.
just got my third cortisone shot this year 😔 the doc said ‘we’ll monitor’ but i know what that means… next time it’s PRP or nothing. 🤞✨
In many traditional healing systems, inflammation is viewed not as an enemy to be suppressed, but as a signal. Suppressing it without addressing root causes may be akin to silencing a smoke alarm while the fire rages. This is not medical advice, merely an observation.
they told me it was safe. they lied. now my shoulder feels like it’s made of wet cardboard and i can’t even reach for my coffee mug. thanks, modern medicine.
I’ve seen this happen too many times. Americans are addicted to quick fixes. You don’t fix a joint with a needle-you fix it with discipline, movement, and accountability. We’re losing our strength because we want a pill, a shot, a gadget. Pathetic.
The biomechanical load redistribution following corticosteroid-induced analgesia often leads to subclinical microtrauma accumulation, particularly in weight-bearing joints. Without concurrent neuromuscular re-education, the risk of structural degradation escalates exponentially.
i’ve had 4 shots in 18 months. the last one made me feel like my knee was filled with broken glass. i’m done. time to learn how to walk again the right way. 🙏
you got this. physical therapy saved my hip. no more needles. just slow, dumb, boring movement. it’s not glamorous but it’s real. you’re not broken-you’re just out of balance. 🏋️♂️💛
The 2023 meta-analysis referenced in the article is methodologically flawed due to heterogeneity in injection protocols, participant selection bias, and lack of standardized outcome measures. Furthermore, the claim that corticosteroids suppress collagen synthesis is overstated-only high-dose, repeated regimens demonstrate this effect, and even then, the clinical significance remains debated.
try yoga first. cheap. free. works.
i used to think shots were magic. then i started walking 30 mins a day. now i can climb stairs without crying. nobody talks about the boring stuff. but the boring stuff is the only thing that lasts. 🌱
This is all a lie. Big Pharma and the AMA are in cahoots. Corticosteroids are designed to make you dependent. They don’t want you healed-they want you coming back every 6 weeks for your next dose. The real cure? Cold laser therapy, magnetic bracelets, and avoiding fluoridated water. I’ve been pain-free for 14 months since I stopped trusting doctors. The system is rigged.
i remember the first time i moved without pain after a shot… it felt like my body remembered how to breathe. but then the pain came back. and i realized-i’d been ignoring my posture, my weight, my fear of movement. the shot didn’t fix me. it gave me a window. i just didn’t walk through it. now i’m trying again. slowly.
did you know the FDA approved Zilretta after a 3-month study funded by the same company that makes the injection? they didn’t test it against physical therapy. they tested it against saline. coincidence? i think not.