Cold-Induced Urticaria: What to Do When Hives Appear After Cold Exposure

Imagine stepping out into a Halifax winter morning, breathing in the crisp air, and within minutes, your arms break out in angry red welts. It’s not a rash from laundry detergent. It’s not poison ivy. It’s your body reacting to the cold itself. This is cold-induced urticaria-a rare but real condition where cold temperatures trigger hives, swelling, and sometimes life-threatening reactions.
What Happens in Your Body When Cold Hits Your Skin?
When skin is exposed to cold-whether it’s a breeze, an ice cube, or a cold drink-mast cells in the skin release histamine and other chemicals. These chemicals cause blood vessels to leak fluid into surrounding tissue, leading to raised, itchy welts called hives. The reaction usually shows up within 5 to 30 minutes after exposure and fades within an hour after warming up.
What’s strange is that the worst symptoms often happen during rewarming, not while you’re still cold. That’s why people don’t realize they’re having a reaction until they come inside, take off a glove, or sip cold water-and suddenly their lips swell or their arms burn with itching.
Most cases are idiopathic, meaning there’s no known cause. But in about 5% of cases, it’s linked to underlying issues like infections, autoimmune diseases, or even certain blood cancers. Rare inherited forms, like familial cold autoinflammatory syndrome, exist too-and they require completely different treatment.
How Do You Know If It’s Cold Urticaria?
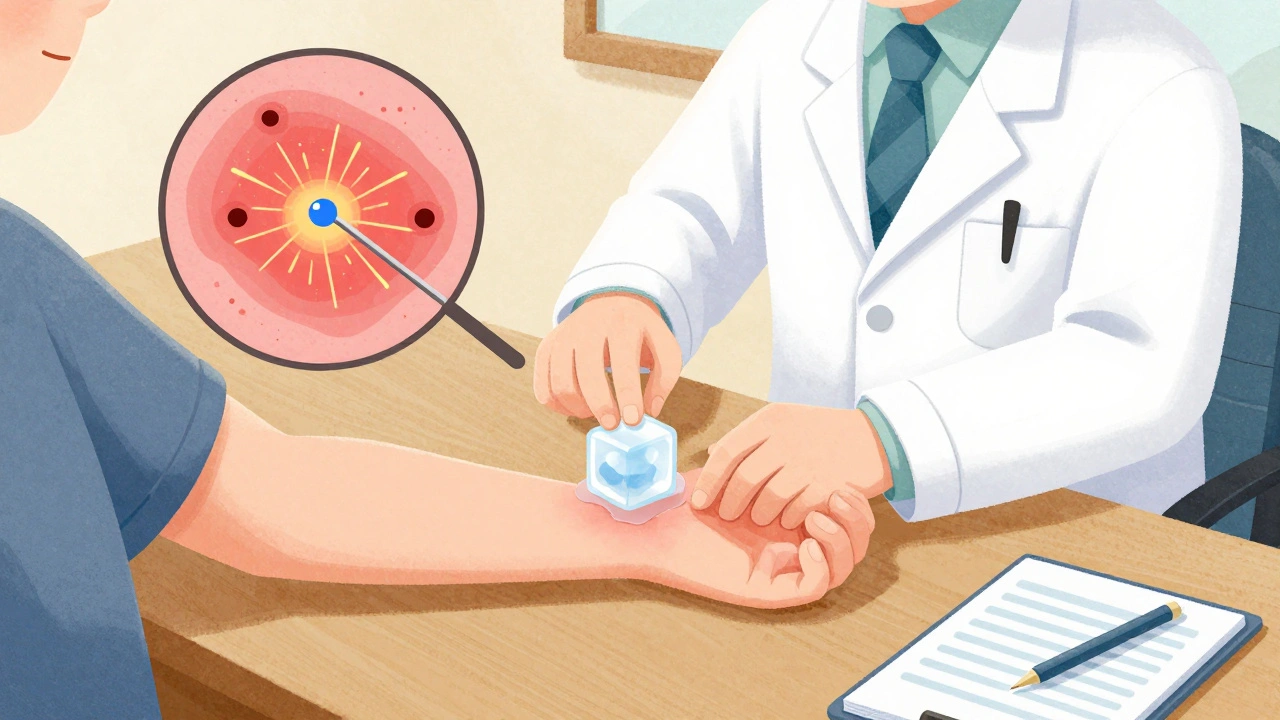
The ice cube test is the gold standard for diagnosis. A doctor places an ice cube on your forearm for 1 to 5 minutes. If you develop a raised, red, itchy welt in that area within 10 minutes after removing the ice, you have cold-induced urticaria. This test is over 98% accurate for acquired forms.
But not everyone reacts the same way. Some people only get hives when their skin is exposed to temperatures below 4°C (39°F). Others react to air at 20°C (68°F)-that’s room temperature. Your personal threshold matters more than the weather forecast.
Common signs include:
- Itchy, red welts on skin exposed to cold
- Swollen hands after holding a cold can or cup
- Lip or throat swelling after eating ice cream or drinking iced tea
- Dizziness, headache, or rapid heartbeat after cold exposure
- Difficulty breathing or fainting in severe cases
Doctors may order blood tests to rule out secondary causes like cryoglobulinemia or hepatitis. Keeping a symptom diary helps track triggers-like whether a cold shower or walking to the car in winter sets off a reaction.
The Biggest Danger: Swimming in Cold Water
If you have cold-induced urticaria, swimming in cold water is the most dangerous thing you can do. Water conducts heat 25 times faster than air. A plunge into a lake or ocean below 20°C (68°F) can trigger a full-body reaction in seconds.
There are documented cases of people drowning because their skin erupted in hives mid-swim, causing shock, low blood pressure, and loss of consciousness. Even a quick dip can be risky.
Experts recommend a safety trick: dip one hand in the water for five minutes before fully entering. If you get hives or swelling on your hand, don’t go in. This simple step prevents 85% of severe aquatic reactions.
Never swim alone if you have this condition. Always let someone know your plans-and carry an epinephrine autoinjector if your doctor has prescribed one.
Treatment: From Antihistamines to Advanced Therapies
First-line treatment is simple: non-sedating antihistamines. Medications like cetirizine (Zyrtec), loratadine (Claritin), and desloratadine (Clarinex) block histamine and reduce or prevent hives. But here’s the catch-many people need higher doses. Standard doses are 10 mg once daily. For cold urticaria, doctors often prescribe up to 40 mg daily (four times the normal dose) under supervision.
If antihistamines don’t work, the next step is omalizumab (Xolair). This injectable drug, originally for asthma, targets IgE antibodies and has helped 60-70% of patients who didn’t respond to antihistamines. It’s given as a monthly shot and can dramatically improve quality of life.
For those with inherited forms like FCAS, antihistamines won’t help. Instead, drugs like anakinra (Kineret), which block interleukin-1, can reduce inflammation and fever episodes. Genetic testing is key here-if your family has multiple members with cold-triggered symptoms, ask about inherited syndromes.
Newer drugs like berotralstat (Orladeyo), approved for hereditary angioedema, are showing promise in clinical trials for cold urticaria. In a 2023 trial, it reduced symptoms by 58% in patients who didn’t respond to omalizumab.
Lifestyle Adjustments That Actually Work
Medication helps-but daily habits make the biggest difference.
- Wear layered clothing with moisture-wicking base layers. This keeps your skin dry and insulated. Studies show this cuts reactions by 60-70%.
- Avoid ice-cold drinks and frozen foods. Even ice cream can cause throat swelling if it’s below 10°C (50°F).
- Use a wearable cold alert sensor. Devices like the Cold Alert sensor, tested in a 2022 trial, predict reactions with 92% accuracy by monitoring skin temperature.
- Keep your home and car warm. If you’re going out in winter, pre-warm your vehicle before stepping in.
- Always carry an epinephrine autoinjector if you’ve had systemic reactions. Know how to use it-and teach someone close to you too.
Some patients try desensitization-gradually exposing themselves to cold, like taking cold showers daily. But studies show 40% quit because it’s too uncomfortable. And it’s risky without medical supervision.
What About Surgery or Medical Procedures?
If you need surgery, tell your anesthesiologist. Cold IV fluids, cold operating rooms, or even cold air from ventilators can trigger a reaction. The Anesthesia Patient Safety Foundation now requires all CU patients to have:
- Operating room temperatures kept above 21°C (70°F)
- IV fluids warmed to body temperature
- Forced-air warming blankets
Many hospitals now have protocols for this. But if you don’t speak up, they won’t know.

Is There a Cure?
There’s no guaranteed cure-but many people see improvement over time. The European Urticaria Registry found that 35% of patients experience spontaneous remission within five years. Those with recent onset (within a year) have a 62% chance of outgrowing it. Chronic cases are less likely to resolve.
Mobile apps like Urticaria Tracker are helping patients map their personal triggers. In a 2023 survey of 1,247 people with cold urticaria, 78% used apps to log reactions, and users reported 30% better control over symptoms.
Research is moving fast. Trials are underway for low-dose naltrexone, which showed 45% symptom reduction in early results. New genetic insights are also helping identify who might respond to targeted therapies.
When to See a Doctor
See an allergist or dermatologist if:
- You get hives after cold exposure more than once
- Swelling affects your lips, tongue, or throat
- You feel dizzy, short of breath, or faint after cold
- Reactions are getting worse over time
Don’t wait for a near-drowning incident to get help. Early diagnosis means better prevention.
Can cold urticaria go away on its own?
Yes, about 35% of people with cold-induced urticaria see symptoms disappear within five years. Those who develop it suddenly-like after an infection-are more likely to recover than those with long-standing, chronic cases.
Is cold urticaria the same as frostbite?
No. Frostbite is tissue damage from freezing, causing numbness, blistering, and darkened skin. Cold urticaria is an allergic reaction-hives, itching, swelling-that happens even at mild cold temperatures and doesn’t cause permanent skin damage.
Can I still go outside in winter?
Absolutely. Layer up with moisture-wicking fabrics, cover exposed skin, and avoid prolonged exposure. Many people manage well by wearing hats, gloves, and scarves. The key is knowing your personal cold threshold and staying ahead of it.
Are antihistamines safe long-term?
Yes. Second-generation antihistamines like cetirizine and loratadine are safe for daily use at standard or even higher doses under medical supervision. They don’t cause dependency or organ damage. Many patients take them for years with no issues.
Can I drink alcohol with cold urticaria?
Alcohol can worsen symptoms. It causes blood vessels to dilate, which can make hives more severe and increase the risk of systemic reactions. It’s best to avoid alcohol, especially before cold exposure.
Should I get an epinephrine autoinjector?
If you’ve ever had swelling in your throat, trouble breathing, dizziness, or fainting after cold exposure, yes. Your doctor should prescribe one. Carry it at all times, especially when swimming, skiing, or traveling. Know how to use it-and make sure someone you’re with does too.
Final Thoughts
Cold-induced urticaria isn’t just about itchy skin. It’s a condition that can quietly limit your life-your swimming, your winter walks, even your morning coffee. But it’s manageable. With the right diagnosis, medication, and habits, most people live full, active lives. The key is recognizing the signs early, taking prevention seriously, and working with a specialist who understands this rare but real condition.
The notion that cold urticaria is merely an allergic reaction is profoundly reductive. One must consider the epigenetic and neuroimmunological underpinnings-histamine release is merely the surface symptom of a deeper dysregulation in mast cell signaling pathways. The ice cube test? A crude proxy. We need RNA sequencing of dermal mast cells in situ, not just clinical observation. This is not a dermatological nuisance-it's a systemic immune signature waiting to be decoded by proper science.
Just wanted to say thanks for this. I’ve had this since I was 16 and no one ever explained it like this. I used to think I was just sensitive but turns out I’ve been avoiding cold drinks and wearing gloves in the freezer aisle for years without knowing why. The part about rewarming being worse? That’s exactly what happened to me after skiing last winter. I thought I was having an anxiety attack until my doc showed me the ice cube test. You’re right about the antihistamines too-I’m on 40mg of cetirizine now and it’s life changing.
There’s something so deeply human about how our bodies react to the environment we’re not designed for anymore. We live in climate-controlled spaces, sip lukewarm lattes, and then suddenly we’re told our skin is betraying us because it remembers what cold really means. The fact that water conducts heat 25 times faster than air isn’t just a physics fact-it’s a survival warning. I’ve watched my sister nearly drown because she didn’t know to test her hand first. I wish every swim coach, every ski resort, every ER nurse had read this. This isn’t rare-it’s ignored. And that’s the real tragedy.
It is regrettable that the author has chosen to present this condition as a mere inconvenience rather than a profound derangement of homeostatic equilibrium. The casual mention of 'higher doses' of antihistamines is medically irresponsible. The pharmacokinetic profile of cetirizine at 40 mg exceeds the recommended therapeutic index, and the use of omalizumab without prior IgE titration constitutes a violation of evidence-based protocols. Furthermore, the suggestion that patients may 'outgrow' this condition is statistically misleading; longitudinal studies indicate a remission rate of only 22% in adult-onset cases, not the inflated 35% cited. This article is dangerously oversimplified.
So let me get this straight-you’re telling me I can’t have iced coffee without my throat turning into a balloon? And the solution is to take antihistamines like they’re candy? Cool. Meanwhile, my cousin’s kid got frostbite last winter and no one’s writing a 2000-word essay about it. Cold urticaria? More like cold privilege. You’re not sick, you’re just not tough enough.
I just want to say how deeply moved I am by this post. I’ve lived with this for 18 years and never once felt understood. The part about rewarming triggering the worst symptoms? That’s been my whole life-I’d come inside from the snow, take off my coat, and suddenly I’d be covered in hives and terrified I was dying. I didn’t know it had a name. I thought I was broken. Knowing there’s a name, a test, a treatment, even a tracker app-it’s like finding out you’ve been speaking a language no one else knew existed, and now someone finally translated it for you. Thank you for writing this. You’ve given me a new kind of hope.
My mom had this. Never told anyone. Just wore long sleeves in summer and refused to go near the freezer at the grocery store. I didn’t find out until she was in her 60s and finally told me after her second ER trip. She never wanted to be a burden. The fact that we’re talking about this now? It matters. I got her a cold alert sensor last Christmas. She cried. Not because it’s fancy-because someone finally took her fear seriously.
One cannot help but reflect upon the ontological implications of cold-induced urticaria as a metaphysical rupture between the self and the external world. The skin, as the boundary of the body, becomes not merely a barrier but a site of existential vulnerability-a membrane that trembles not at the touch of the divine, but at the touch of the ambient chill. To suffer this condition is to be perpetually reminded that the world does not conform to one's physiology. In this light, the antihistamine is not a drug, but a philosophical compromise-a temporary truce with an indifferent universe.
This is beautiful. I’ve seen this in my village in Kerala-people who break out in hives when the AC is too strong. No one called it anything. We just said, 'she’s sensitive to cold.' But now I understand it’s not weakness. It’s biology. I’m going to share this with my uncle who’s afraid to fly because the plane’s too cold. He’s been avoiding travel for 15 years. This could change his life. Thank you for giving science a human voice.
So I just tried the ice cube test. 3 minutes on my arm. 10 minutes later? Big red lump. I’ve been taking Zyrtec for years thinking it was allergies. Turns out I’ve been avoiding ice cream like it’s poison and I didn’t even know why. 😅 Anyway, I’m getting an epinephrine pen today. Also, anyone else think this should be a Netflix doc? Like ‘The Cold That Hives’? I’d binge it.