Carbohydrate Counting for Diabetes: A Complete Beginner’s Guide

Managing diabetes isn’t about cutting out carbs entirely-it’s about knowing exactly how much you’re eating and how it affects your blood sugar. That’s where carbohydrate counting comes in. It’s not a diet. It’s not a restriction. It’s a practical tool that gives you control. And if you’re new to it, you’re not alone. Millions of people with diabetes use carb counting every day to keep their numbers stable, avoid spikes, and eat the foods they love-without guesswork.
Why Carbohydrate Counting Matters
Carbs turn into glucose-the main fuel your body uses. For someone without diabetes, insulin handles this smoothly. But if you have type 1 or type 2 diabetes (especially if you take insulin), your body doesn’t manage that glucose properly. Too many carbs at once? Blood sugar shoots up. Too few? You risk low blood sugar. Carb counting helps you match what you eat with the insulin you need.The American Diabetes Association (ADA) calls carb counting an evidence-based method. Studies show people who track their carbs regularly see HbA1c drops of 0.5% to 1.0%-a big deal when your goal is below 7%. It’s not magic. It’s math. And once you learn it, you’ll notice fewer highs and lows, less fatigue, and more confidence in your daily choices.
How Carbs Work: The 15-Gram Rule
All carbs are measured in grams. One standard serving equals about 15 grams of total carbohydrates. That’s the baseline. Think of it like a unit. Once you know what 15 grams looks like, you can add them up.Here are common foods that equal one 15-gram carb serving:
- 1 small apple (about 4 ounces)
- 1 slice of bread
- 1/2 cup of cooked rice or pasta
- 1/2 cup of beans or lentils
- 1 cup of milk
- 1/3 cup of oatmeal
- 1 small tortilla
Notice how some of these are fruits, grains, dairy, and legumes? Carbs aren’t just bread and pasta. They’re in yogurt, milk, starchy veggies like potatoes and corn, and even some sauces. That’s why counting matters-you can’t eyeball it.
Reading Labels Like a Pro
Nutrition labels are your best friend. Look for “Total Carbohydrates.” That number includes sugars, starches, and fiber-all of it. But here’s the trick: you don’t always count it all.If the label says “Dietary Fiber” is 5 grams or more, subtract the full amount. Fiber doesn’t raise blood sugar. So if a food has 20 grams of total carbs and 6 grams of fiber, you count only 14 grams.
Sugar alcohols? They’re in sugar-free gum, candies, and some low-carb products. Subtract half their amount. If a product has 10 grams of sugar alcohol, subtract 5 grams from the total carbs.
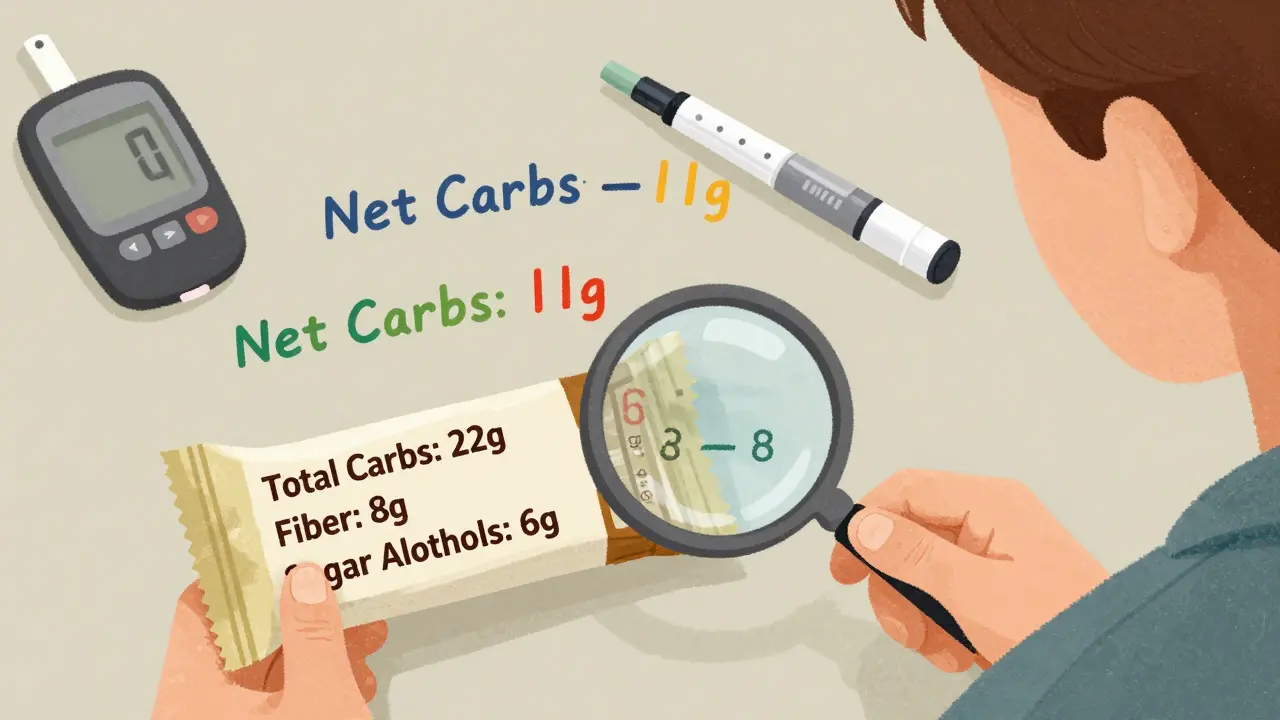
Example: A protein bar says:
- Total Carbohydrates: 22g
- Dietary Fiber: 8g
- Sugar Alcohols: 6g
Net carbs = 22 - 8 - (6 ÷ 2) = 22 - 8 - 3 = 11 grams.
That’s the number you use for insulin dosing or tracking.
Matching Carbs to Insulin: The Ratio
If you take insulin, you need a carb-to-insulin ratio. This tells you how many units of insulin to take per gram of carbs. It’s personal. One person might need 1 unit for every 10 grams of carbs. Another might need 1 unit for every 15 grams.Your doctor or diabetes educator will help you figure this out. It’s based on your weight, activity, insulin type, and how your body responds. Start with what they recommend. Then use your glucose meter or CGM to see how you respond after meals.
Example: Your ratio is 1:10. You eat a sandwich with 45 grams of carbs. 45 ÷ 10 = 4.5 units of insulin. Round to 4.5 or 5, depending on your doctor’s advice.
Don’t forget: your ratio might change. You might need more insulin at breakfast than dinner. That’s normal. Your body’s insulin sensitivity shifts throughout the day.
Carb Counting vs. Other Methods
You might have heard of the plate method or glycemic index (GI). Here’s how carb counting stacks up:- Plate Method: Fill half your plate with non-starchy veggies, a quarter with protein, a quarter with carbs. Simple, but no numbers. Good for beginners, but doesn’t help with insulin dosing.
- Glycemic Index: Rates carbs by how fast they raise blood sugar. Low-GI foods are slower. But it ignores portion size. Eating a large amount of low-GI food still spikes blood sugar.
- Carb Counting: Gives you exact numbers. Lets you eat anything, as long as you adjust insulin. Best for people on insulin pumps or multiple daily injections.
Carb counting is the most precise tool for insulin users. If you’re on pills only, you might not need it-but it still helps you understand how food affects you.
Tools You Need to Start
You don’t need fancy gear. But these tools make it easier:- Food scale: Weighing portions is the most accurate way. A $15 kitchen scale works.
- Measuring cups and spoons: For rice, pasta, cereal, yogurt.
- Calculator or app: Use MyFitnessPal, Carb Manager, or the free USDA FoodData Central app. Scan barcodes or search foods.
- Food diary: Write down everything you eat, with portion sizes and insulin doses. Review with your doctor every few weeks.
Most people spend 30-60 minutes per meal the first month. That’s normal. After 3-4 weeks, estimating becomes second nature.
Common Mistakes (and How to Avoid Them)
Here’s what trips up beginners:- Forgetting hidden carbs: Milk in coffee, sauce on pasta, fruit in yogurt. These add up fast. Track them.
- Estimating restaurant meals: Chains list carbs online. Use their nutrition pages. If unsure, assume 20-30% more than labeled.
- Ignoring fiber and sugar alcohols: Always check the label. Don’t just look at “sugars.”
- Not adjusting for activity: Exercise lowers blood sugar. If you’re active, you may need less insulin for the same carbs.
- Skipping meals: Skipping carbs without adjusting insulin leads to lows. Consistency matters.
One user on Reddit said: “My post-meal spikes dropped from 250+ to 160-180 in two weeks. I just started measuring everything.” That’s the power of accuracy.
Real Progress: What Success Looks Like
Success isn’t perfection. It’s consistency.One patient, tracked for 18 months, dropped their HbA1c from 8.9% to 6.2%. They didn’t eat “diabetic food.” They ate pizza, pasta, and ice cream-but counted every gram and matched insulin. That’s the point.
People who stick with carb counting report:
- More stable energy throughout the day
- Fewer hospital visits for highs or lows
- More freedom to eat out or travel
- Less anxiety about food
It’s not about being perfect. It’s about being aware.

What’s New in Carb Counting (2026)
The science hasn’t changed-but the tools have.- AI food scanners: Apps like Carb Manager’s SmartScan use your phone camera to estimate carbs from photos. Accuracy is around 85%.
- Smart insulin pens: Some pens now sync with apps to log doses and carbs automatically.
- Integrated CGMs: Continuous glucose monitors show you real-time how your body reacts to specific meals. You can see if your carb count was off within minutes.
- Updated USDA database: Over 300,000 foods, updated quarterly. Includes restaurant items and international foods.
The goal? Make carb counting faster, easier, and more accurate. You’re not fighting your food-you’re understanding it.
When You Might Not Need It
Carb counting isn’t for everyone. If you have type 2 diabetes and manage with diet, exercise, and oral meds (like metformin), you might do fine with portion control or the plate method.But even then, knowing your carb intake helps. If your blood sugar is still high, you’ll know if it’s because of rice, bread, or fruit. You’ll have data, not guesswork.
And if you ever start insulin? You’ll be ready.
Next Steps: How to Start Today
1. Get a food scale and measuring cups. Buy them online or at a dollar store. 2. Track everything for 3 days. Write down every bite, every sip. Use an app or paper. 3. Find your average daily carb intake. Add it up. If you’re eating 300 grams a day, you’re in the typical range. Most adults with type 1 diabetes need 150-250 grams. 4. Learn your 15-gram portions. Measure a slice of bread, a cup of milk, a banana. See what it looks like. 5. Ask your doctor for your carb-to-insulin ratio. If you don’t have one, get one. 6. Use an app. MyFitnessPal or Carb Manager. Scan barcodes. Log meals. Check your numbers. 7. Review with your diabetes educator. Bring your log. They’ll help you adjust.You don’t need to be perfect. You just need to start.
Do I have to count carbs if I’m on insulin?
Yes-if you take mealtime insulin, counting carbs is essential. Insulin doesn’t work unless you match it to the carbs you eat. Without counting, you risk highs, lows, or unpredictable swings. Even if you’re on a pump, you still need to input carb amounts for accurate dosing.
Can I eat sweets while carb counting?
Absolutely. Carb counting gives you flexibility. A cookie, a slice of cake, or a scoop of ice cream? Count the carbs, match the insulin, and enjoy it. The goal isn’t to eliminate treats-it’s to include them safely. Many people with diabetes say this freedom is what makes carb counting sustainable long-term.
What if I forget to count carbs at a restaurant?
Check the restaurant’s nutrition info online before you go. Most chains list carbs. If you can’t find it, estimate conservatively-assume 20-30% more than you think. If you’re unsure, take half your usual insulin dose, then check your blood sugar 2 hours later. If it’s high, you can correct with a small insulin dose. Never skip insulin just because you didn’t count.
How long does it take to get good at carb counting?
Most people reach 85% accuracy after 30 days of consistent tracking. The first week is the hardest-you’ll measure everything. By week 3, you’ll start recognizing portions by sight. After 2 months, you’ll estimate most meals without tools. It’s a skill, not a test. Progress, not perfection, is the goal.
Do I still need to count carbs if I use a CGM?
Yes. A CGM shows you what happened-but not why. It tells you your blood sugar spiked after lunch. Carb counting tells you it was because of the 60 grams of rice you ate. You need both: the data from your CGM and the control from carb counting. Together, they give you full power over your diabetes.
I started carb counting last year after my HbA1c hit 8.4. Honestly? Life changed. I still eat pizza on Fridays. Just count the damn carbs and dose accordingly. No guilt, no magic, just math.
Also, that 15g rule? Game changer. I used to eyeball everything and wonder why I was crashing by 3pm. Now I know exactly what I'm working with.
Carb counting...? How quaint. In my country, we simply eat whole foods, avoid processed sugar, and let nature regulate insulin. The ADA’s obsession with grams is a pharmaceutical industry puppet show. Fiber? Sugar alcohols? You’re being manipulated into overcomplicating a simple biological process.
Let me guess - you’re also telling people to trust nutrition labels from corporations that lobbied to hide trans fats for decades. The USDA database? Updated quarterly? Ha. They still list ‘fruit-flavored yogurt’ as 15g carbs when it’s actually 32g with added syrups. This whole system is a placebo for people too scared to question the system.
I appreciate the clarity of this guide - especially the breakdown of net carbs. I’ve been using carb counting for five years, and I still find myself overestimating fiber in whole grain breads. The key, I’ve learned, is consistency over perfection. It’s not about being right every time - it’s about building awareness.
Also, the part about insulin sensitivity shifting throughout the day? So true. My ratio at breakfast is 1:8. At dinner? 1:14. It took me months to notice the pattern.
i luv this post!! i just got diagnoised with type 2 and was so scared but this made me feel like i can do it!! thanks!!
Man, I used to think carbs were the enemy. Then I ate a whole bag of chips, didn’t count, and spiked to 310. Next day? I measured a single apple - 15g. A slice of toast - 15g. Suddenly, it wasn’t about deprivation. It was about dance. Food and insulin, waltzing together. I’m not a robot. I’m not a diet. I’m a human who eats, moves, and adjusts. And that’s okay.
They don’t want you to know this but CGMs are controlled by Big Pharma to keep you hooked on insulin. The real solution is keto. No carbs. No insulin. No lies. Why do you think they push carb counting? So you keep buying insulin pens and apps. Wake up.
The assumption that all fiber is non-digestible is scientifically flawed. Soluble fiber can still impact glycemic response, particularly in individuals with gastroparesis. Furthermore, the 5g threshold for fiber subtraction is arbitrary and not universally applicable. This guide dangerously oversimplifies metabolic physiology.
They’re hiding the truth. The real reason carb counting works is because it makes you dependent on insulin. If you just ate low-carb, you wouldn’t need it. But then they’d lose billions. The ADA, the FDA, the food industry - all in cahoots. Your ‘15g serving’? It’s a trap. Your CGM? A surveillance tool. You’re being monitored.
There’s a quiet beauty in measuring your life in grams. Not just carbs - but moments. The way you pause before eating. The way you check your meter not out of fear, but curiosity. It’s not control. It’s communion. You’re not fighting your body. You’re listening to it. And in that listening? You find freedom.
I’ve been doing this for three years. The first month was brutal. I measured everything. I hated it. But now? I can walk into a Thai restaurant, glance at the pad thai, and know it’s 60g carbs. I don’t stress. I don’t panic. I just adjust. It’s not perfect. But it’s mine. And that’s enough.
I don’t trust any of this. What if the apps are hacked? What if the food labels are wrong? What if the CGM is lying? I’ve had three false highs because of ‘calibration errors.’ They told me to ‘trust the data’ - but who’s really in control? I’m just trying to survive, not become a data point.