Antiviral Medications and CYP3A4/P-glycoprotein Interactions: What You Need to Know
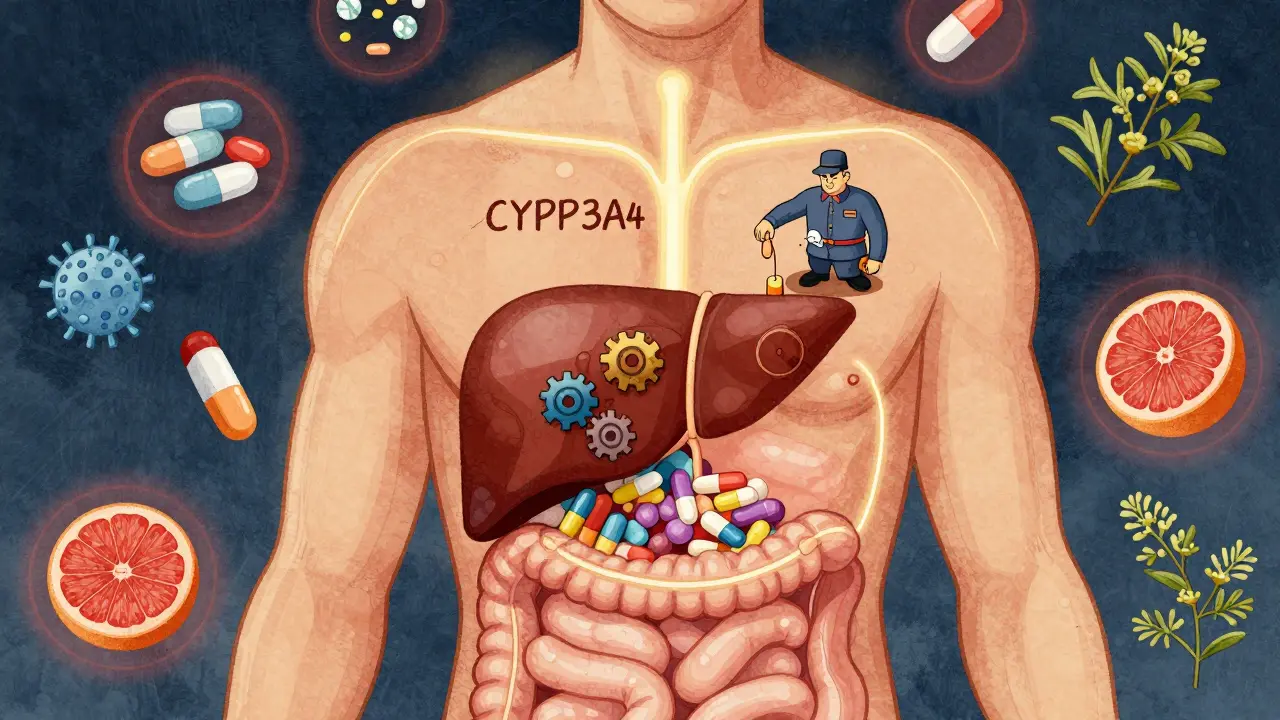
When you’re taking antiviral meds like those for HIV or hepatitis C, it’s not just about the drug itself. What you’re also taking - whether it’s a statin, a blood thinner, or even grapefruit juice - can make the difference between treatment working and landing in the hospital. Two hidden players in this game are CYP3A4 and P-glycoprotein (P-gp). These aren’t just buzzwords. They’re biological gatekeepers that control how much of your medication actually gets into your bloodstream - and how fast it gets cleared out.
What Are CYP3A4 and P-glycoprotein?
CYP3A4 is the most common enzyme in your liver and gut that breaks down drugs. About half of all medications you take - including many antivirals - go through this system. Think of it like a factory that chops up chemicals so your body can flush them out. Then there’s P-glycoprotein, a transporter protein that acts like a bouncer at the door of your cells. It kicks drugs out before they can be absorbed, especially in your intestines, brain, and kidneys. Together, they decide whether a drug works, causes side effects, or doesn’t work at all.
These systems became a big deal in antiviral therapy after ritonavir, an HIV drug approved in 1996, was found to shut down CYP3A4. Doctors realized they could use tiny doses of ritonavir - just 100 mg - to block the enzyme and make other antivirals last longer in the body. That’s how “boosting” was born. Today, ritonavir and its cousin cobicistat are used as pharmacokinetic boosters in drugs like Kaletra, Prezcobix, and Evotaz. But here’s the catch: while boosting helps antivirals work better, it also makes your body more sensitive to everything else you’re taking.
Why These Interactions Are Dangerous
Imagine you’re on apixaban (Eliquis) for blood thinning and start a new HIV regimen with darunavir/cobicistat. Both are processed through CYP3A4 and P-gp. The antiviral blocks the enzyme and transporter, so apixaban doesn’t get broken down. Your blood levels of apixaban can spike - by up to 300% in some cases. That’s not just a lab number. That’s internal bleeding risk. A 2021 case report in the Journal of Acquired Immune Deficiency Syndromes described a 68-year-old man who bled internally after starting this combo. His anti-Xa levels hit 384 ng/mL. The safe range? 50-250.
Or take simvastatin, a common cholesterol drug. When taken with the hepatitis C combo paritaprevir/ritonavir/ombitasvir/dasabuvir, simvastatin levels jump 1,760%. That’s not a typo. That’s enough to cause rhabdomyolysis - a condition where muscle tissue breaks down and can lead to kidney failure. The FDA warns against this combo outright.
Even herbal supplements can mess with this system. St. John’s wort - often used for mild depression - can slash ritonavir levels by 57%. That means your HIV meds might not work. Grapefruit juice? It does the opposite. It boosts ritonavir by 23% by blocking CYP3A4 in your gut. One glass might not kill you, but daily? That’s a slow-motion overdose waiting to happen.
How Different Antivirals Compare
Not all antivirals are created equal when it comes to interactions. Ritonavir is the heavyweight champion of drug interactions - powerful, but messy. It doesn’t just inhibit CYP3A4; it also induces CYP1A2, which can lower levels of drugs like olanzapine (an antipsychotic) by 29%. That’s why some patients on ritonavir don’t see expected interactions - because opposing effects cancel out.
Cobicistat, introduced later, is cleaner. It doesn’t induce CYP1A2, so fewer competing effects. But it’s stronger at inhibiting UGT1A1, which can raise bilirubin levels and make your skin look yellow - harmless, but alarming. It also blocks OCT2, a kidney transporter, leading to higher creatinine levels. That doesn’t mean kidney damage, but it can trick doctors into thinking you have kidney disease.
For hepatitis C, newer regimens like glecaprevir/pibrentasvir are far safer. Only 17% of common medications need dose changes with this combo. Compare that to older regimens like paritaprevir/ritonavir/ombitasvir/dasabuvir - where 42% of medications require adjustment. Even so, all DAAs (direct-acting antivirals) are P-gp substrates. That means if you take something that blocks P-gp - like verapamil or cyclosporine - your antiviral levels can skyrocket.
And then there’s sofosbuvir. It barely touches CYP3A4, so it’s great for people on multiple meds. But it’s still a P-gp substrate. So even if you’re not on a boosted regimen, you still need to watch for transporter interactions.

Real-World Consequences
In 2021, a study of nearly 5,000 HIV and hepatitis C patients across Europe found that 17.3% of adverse drug events were due to uncaught interactions. That’s one in six people having a bad reaction because no one checked what else they were taking.
One patient on warfarin (a blood thinner) started ritonavir-boosted antivirals. His INR - a measure of blood clotting - went from 2.1 to 7.8 in two weeks. He ended up in the ER with a brain bleed. Four out of twelve similar cases in a 2021 case series required hospitalization.
But it’s not all doom and gloom. A 2022 study with 347 HIV patients showed that using the free University of Liverpool HIV Drug Interactions Checker app dropped interaction-related problems from 18.7% to just 5.2% in 12 months. That’s a 72% reduction. The app flags risky combos with color codes: green = safe, yellow = monitor, red = avoid. It’s used by over a million people worldwide.
Still, many patients feel trapped. On Reddit, someone wrote: “My psychiatrist won’t prescribe me anything for anxiety because of my darunavir regimen - it’s like choosing between mental health and viral suppression.” That’s the human cost. We’re so focused on suppressing the virus that we forget the person taking the pills.
How to Stay Safe
There’s a simple, three-step process every patient and provider should follow:
- Make a full list - every pill, patch, supplement, and herbal product. Don’t forget OTC meds like ibuprofen or melatonin. Even vitamins can interfere.
- Check with a reliable tool - Use the Liverpool HIV Interactions Checker (free, web and app versions). It’s validated against expert panels and has 98.7% accuracy.
- Talk to your pharmacist - Pharmacists are trained in drug interactions. They see your full med history. Ask them: “Could any of these meds be making my antiviral too strong or too weak?”
Timing matters too. Some clinicians delay starting anticoagulants or statins for a month after beginning antiviral therapy. That lets the new drug reach steady state before adding another. It’s not always necessary, but in high-risk cases, it’s a smart buffer.
Also, don’t assume your doctor knows everything. FDA labels give you the data, but they rarely tell you what to do. The European Association for the Study of the Liver (EASL) guidelines do - but you need to access them. Most clinics in Europe use screening protocols. In the U.S., only 68% do. If your provider hasn’t asked you about all your meds, ask them why.

The Future: Personalized Antiviral Therapy
What’s next? Pharmacogenomics. Your genes can tell you how you’ll handle these drugs. For example, if you have the CYP3A5*3/*3 genotype - common in 85% of Caucasians - you’re a slow metabolizer. When you take ritonavir with tacrolimus (an immunosuppressant), your tacrolimus levels can be 2.3 times higher than normal. That’s not a guess. That’s from a 2023 study. Genetic testing isn’t routine yet, but it’s coming.
Meanwhile, new antivirals like lenacapavir are being designed to avoid CYP and transporter systems entirely. That’s the goal: drugs that work without messing with your other meds. But with 39 million people on antiretrovirals by 2025 - and most of them over 50 with multiple chronic conditions - we’re not there yet.
As Dr. Melanie Thompson said at the 2023 Retroviruses Conference: “The next frontier isn’t the virus. It’s managing the 4.7 average comorbidities per person with HIV. CYP and transporter interactions will decide if treatment succeeds - not viral load.”
Bottom Line
Antiviral meds save lives. But they don’t live in a vacuum. CYP3A4 and P-glycoprotein are silent gatekeepers. One wrong combo can cause bleeding, muscle damage, kidney failure, or treatment failure. The good news? You don’t need to be a doctor to protect yourself. Know your meds. Use the Liverpool app. Talk to your pharmacist. And don’t let anyone tell you it’s “just a supplement” or “a little grapefruit juice.” In this game, small things have big consequences.
This is one of those posts that makes you realize how little you actually know about your own meds. I’ve been on HIV treatment for six years and never thought about grapefruit juice being a silent saboteur. Now I check every new supplement like it’s a landmine. Thanks for laying it out so clearly.
Let me tell you - I was on simvastatin for years. Then my doctor switched me to a boosted regimen and suddenly I couldn’t lift my arms. Muscle pain so bad I cried walking up stairs. They didn’t even connect it until my creatine kinase was through the roof. This isn’t theoretical. It’s life-altering. Please, if you’re on antivirals, treat your med list like a bomb squad checklist.
Why are we letting Big Pharma design drugs that require a PhD to use safely? This is a scam. They know the interactions are deadly, but they don’t care as long as the prescriptions keep flowing. Wake up, people.
As someone who grew up in Nairobi and now lives in Atlanta, I’ve seen how different healthcare systems handle this. In Kenya, most people just take what’s given and hope. Here, we have the Liverpool app - free, accurate, and easy. But only if you know it exists. I’ve shared it with three friends already. Knowledge isn’t power - it’s survival.
Ugh. Another wall of text. Can we just say: don’t mix drugs with juice? Why do we need 10 paragraphs to say grapefruit is bad? And why does everyone act like this is new? My grandma knew this in the 90s. Stop overcomplicating things.
While the Liverpool app is certainly useful, it is, in my view, an inadequate palliative for a broken pharmacological infrastructure. The reliance on external tools to mitigate the consequences of poorly designed drug interactions speaks to a systemic failure - one that prioritizes profit over physiological coherence. One must ask: who benefits from this complexity? And why are we still using CYP3A4-dependent scaffolds in 2024?
they say cyp3a4 and p-gp but what if it’s all a lie? what if the gov and big pharma made this up so we’d take more pills? i read somewhere that the liver doesn’t even work like they say… and what about that guy who drank grapefruit juice for 20 years and never got sick? they’re lying. they always lie.
THIS IS WHY YOU NEED TO BE CAREFUL 😰 I had a friend on PrEP + Adderall + statin - all three got boosted by the antiviral. He ended up in the ER with chest pain and a heart rate of 140. They thought it was a heart attack. Turned out it was just drug overload. I told him to use the Liverpool app. He didn’t. Now he’s fine… but barely. 🙏 Don’t be him.