Antibiotic-Related Liver Injury: Understanding Hepatitis and Cholestasis Risks
Liver Injury Pattern Calculator
Calculate the R-ratio (ALT/ALP) to determine the type of liver injury caused by antibiotics. This tool helps identify if the injury is hepatitis (ALT > 5x normal), cholestasis (ALP > 2x ALT), or mixed pattern.
Interpretation Guide
- R > 5: Hepatitis (liver cells damaged)
- R < 2: Cholestasis (bile flow blocked)
- 2 ≤ R ≤ 5: Mixed pattern
Note: R = ALT / ALP
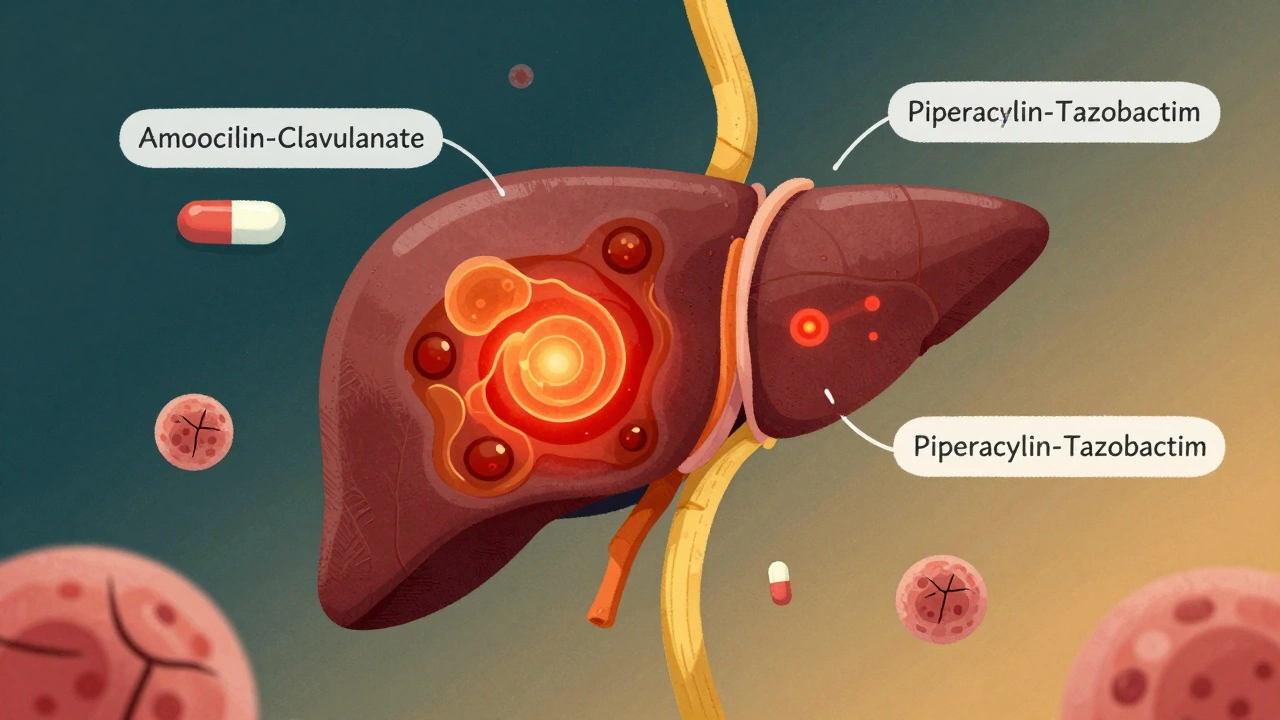
Antibiotics save lives, but they can also quietly damage the liver. For every 100,000 prescriptions of amoxicillin-clavulanate, 15 to 20 people will develop serious liver injury. That’s not rare. It’s common enough that doctors need to watch for it-especially when patients are on antibiotics for more than a week. The liver doesn’t always scream when it’s hurt. Sometimes, the only sign is a slightly elevated blood test. Other times, the skin turns yellow, the belly aches, and the person feels too tired to get out of bed. This isn’t just a side effect. It’s a real, measurable risk tied to specific drugs, dosing, and even genetics.
How Antibiotics Hurt the Liver
Antibiotics don’t attack the liver on purpose. They’re meant to kill bacteria. But sometimes, the way they’re broken down in the body creates toxic byproducts. These toxins overload liver cells, damage mitochondria (the energy factories inside cells), and trigger inflammation. The result? Two main patterns of injury: hepatitis and cholestasis.
Hepatitis means liver cells are dying. Blood tests show ALT (alanine aminotransferase) levels above five times the normal limit. This is the body’s alarm bell that liver cells are being destroyed. Cholestasis is different. It’s when bile can’t flow out of the liver. Alkaline phosphatase (ALP) rises sharply, and bilirubin builds up, causing jaundice. The R-ratio helps doctors tell them apart: if ALT is much higher than ALP (R > 5), it’s hepatitis. If ALP is way higher than ALT (R < 2), it’s cholestasis. If it’s in between, it’s mixed.
Some antibiotics almost always cause cholestasis. Amoxicillin-clavulanate is the classic example-70 to 80% of its liver injuries are cholestatic. Others, like ciprofloxacin and azithromycin, tend to cause mixed patterns. Meanwhile, tazobactam/piperacillin, a common ICU drug, causes liver injury in nearly 3 out of 10 patients who get it for more than seven days. That’s not a fluke. It’s a pattern.
Who’s Most at Risk?
Not everyone who takes antibiotics gets liver damage. But some people are far more likely to. The biggest risk factor? Time. Taking antibiotics for seven days or longer increases the chance of liver injury by more than three times. That’s why a simple 5-day course of amoxicillin is low risk, but a 14-day IV drip of piperacillin in the ICU is dangerous.
Another hidden risk is sepsis. Patients already fighting a severe infection are 1.8 times more likely to develop antibiotic-related liver injury. Why? Their livers are already stressed. Adding a toxic drug on top pushes them over the edge. Gender matters too. Men are 2.4 times more likely than women to get liver damage from meropenem. And genetics? That’s the new frontier. Certain HLA gene variants make some people extra sensitive to drugs like amoxicillin-clavulanate. It’s not about dose-it’s about who you are.
Older adults, people with existing liver disease, and those on multiple medications are also at higher risk. But even healthy young people can be affected. That’s why it’s so hard to spot. The symptoms-nausea, fatigue, dark urine-look like the infection itself. In the ICU, it’s easy to blame the sepsis, not the antibiotic.
Which Antibiotics Are the Worst Offenders?
Some antibiotics are far more dangerous to the liver than others. The LiverTox database, maintained by the U.S. National Institutes of Health, ranks them by risk. Amoxicillin-clavulanate is in the highest-risk category (score 8-10). It’s the most common cause of antibiotic-related liver injury in the U.S.
Here’s how the top offenders compare:
| Antibiotic | Primary Injury Pattern | Incidence per 100,000 Prescriptions | Typical Onset Time | Risk Category (LiverTox) |
|---|---|---|---|---|
| Amoxicillin-clavulanate | Cholestatic | 15-20 | 1-6 weeks | High (8-10) |
| Tazobactam/piperacillin | Mixed | 12-18 (in ICU) | 1-3 weeks | High (8-10) |
| Nitrofurantoin | Hepatocellular | 3-5 | 1-8 weeks | Moderate (5-7) |
| Trimethoprim-sulfamethoxazole | Mixed | 2-4 | 1-4 weeks | Moderate (5-7) |
| Ciprofloxacin | Mixed | 1-3 | 1-2 weeks | Moderate (5-7) |
| Meropenem | Hepatocellular | 1-2 | 1-3 weeks | Low (1-4) |
Even drugs like rifampin and isoniazid-used for tuberculosis-can cause serious liver damage, especially when taken together. And while meropenem is generally safer, it still causes injury in 12% of long-term ICU patients, mostly men. The takeaway? Not all antibiotics are created equal. Some are safer than others, but none are risk-free.

How Doctors Spot the Problem
There’s no single test for antibiotic-induced liver injury. It’s a diagnosis of exclusion. That means doctors have to rule out other causes: viral hepatitis, alcohol, gallstones, heart failure, or even the infection itself. In the ICU, this is especially hard. Patients are often on 5 or 6 different drugs. Their livers are already struggling.
So what do they look for? First, timing. Did the liver enzymes rise after starting the antibiotic? Did they drop after stopping it? That’s a strong clue. Second, the pattern. Is ALT sky-high? That’s hepatitis. Is ALP elevated with jaundice? That’s cholestasis. Third, symptoms. Nausea, itching, dark urine, pale stools-these matter. A patient with a 6× ALT and no symptoms might just be monitored. But if they’re jaundiced and vomiting, the antibiotic must stop.
Most hospitals follow the "rule of 5": stop the drug if ALT is over 5× normal, or if ALP is over 2× normal with symptoms. But some clinics are more cautious. Others wait for bilirubin to rise. There’s no universal rule-just guidelines.
What to Do If You’re on Antibiotics
If you’re prescribed a high-risk antibiotic like amoxicillin-clavulanate or piperacillin-tazobactam, ask your doctor about liver monitoring. Baseline blood tests before starting are essential. Then, get tested again after 7 to 10 days. For long courses, weekly checks are recommended. Don’t wait for symptoms. By the time you feel bad, the damage may already be done.
Don’t assume your primary care doctor will catch it. Studies show only 3-5% of cases are spotted in outpatient settings. In hospitals, it’s better-8-12% of ICU patients are monitored closely. But even then, many cases are missed. If you’re on antibiotics for more than a week and start feeling unusually tired, nauseous, or notice your eyes turning yellow, speak up. Bring your lab results. Ask: "Could this be the antibiotics?"
For now, the best protection is awareness. Know your drug. Know your risk. Know your numbers.
What’s Next? New Tools and Hope
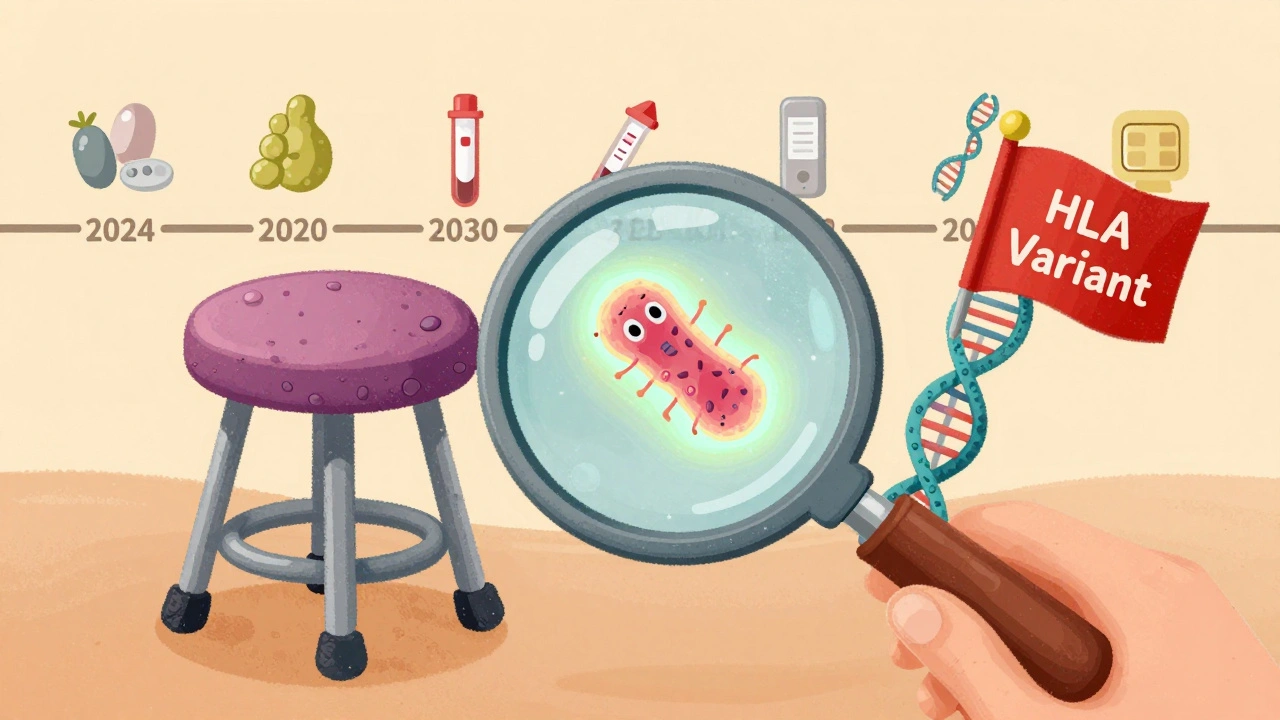
Science is catching up. Researchers are now looking at the gut microbiome to predict who’s at risk. A drop in one specific bacteria-Faecalibacterium prausnitzii-is linked to a 3.7-fold higher chance of liver injury. Soon, a simple stool test might tell you if your body is primed for trouble.
Clinical trials are testing probiotics to protect the gut and liver during antibiotic treatment. Early results are promising. Meanwhile, genetic testing for HLA variants could one day let doctors avoid high-risk drugs for sensitive patients. Within five to seven years, we may be able to personalize antibiotic choices based on your DNA.
For now, the tools are simple: know the drugs, monitor the liver, stop early if needed. The goal isn’t to avoid antibiotics. It’s to use them wisely. Because when the liver gets hurt, recovery can take months-even if the infection is gone.
Can antibiotics cause permanent liver damage?
In most cases, no. If the antibiotic is stopped early and the injury is caught in time, the liver usually heals completely within weeks to months. But in rare cases-especially if the drug is continued despite rising enzymes or jaundice-acute liver failure can occur. This may require a transplant. The risk is low, but it’s real. That’s why monitoring matters.
Are over-the-counter antibiotics linked to liver injury?
In the U.S., antibiotics are prescription-only. But in some countries, they’re sold without a prescription. Even then, the risk comes from the same drugs: amoxicillin-clavulanate, nitrofurantoin, trimethoprim-sulfamethoxazole. The danger isn’t whether it’s OTC or prescription-it’s whether the drug is high-risk and taken for too long.
How long does it take for liver enzymes to return to normal after stopping the antibiotic?
It varies. For mild cases, ALT and ALP often drop by half within 2 weeks. Full recovery usually takes 4 to 12 weeks. If bilirubin was elevated, it can take longer-up to 6 months. Persistent elevation beyond 3 months should be investigated for other causes.
Can I take acetaminophen (Tylenol) if I have antibiotic-related liver injury?
Avoid it. Acetaminophen is processed by the liver and can add stress when the organ is already damaged. Even at normal doses, it may worsen injury. Use alternatives like ibuprofen if approved by your doctor. Always check with your provider before taking any new medication.
Do natural supplements help protect the liver during antibiotic use?
There’s no strong evidence that milk thistle, turmeric, or other supplements prevent antibiotic liver injury. Some may even interact with antibiotics or worsen liver stress. Probiotics show promise in clinical trials, but only specific strains are being studied. Don’t rely on supplements-rely on monitoring and stopping the drug if needed.
Bottom Line
Antibiotic-related liver injury isn’t rare. It’s common, underrecognized, and preventable. The drugs that save you can also hurt you-especially if you’re on them too long or have other health risks. Know the signs. Ask for blood tests. Speak up if something feels off. Your liver doesn’t have a voice. You have to speak for it.
Bro this is wild. I was on amoxicillin-clavulanate for a sinus infection last year and felt like death for three weeks. No one even checked my liver enzymes. My doctor just said 'it's probably the bug.' Bullshit. My ALT was through the roof. They should be testing everyone on long courses, not waiting for jaundice.
It's crazy how we treat antibiotics like candy. Like, 'oh it's just a pill,' but they're basically chemical grenades in your bloodstream. I've seen ICU nurses quietly panic when someone's on piperacillin-tazobactam for more than five days. The liver doesn't scream until it's too late. Maybe we need a little red flag on the prescription label: 'This might quietly murder your liver.' Just saying.
It is axiomatic that pharmacological agents, by virtue of their metabolic transformation, invariably generate bioactive byproducts which may exert hepatotoxic effects. The pathophysiological dichotomy between hepatocellular and cholestatic injury, as delineated by the R-ratio, constitutes a fundamental paradigm in clinical pharmacology. The temporal association between drug administration and enzyme elevation remains the cornerstone of diagnostic inference, though confounding variables-particularly in polypharmacy contexts-necessitate rigorous exclusionary protocols.
I had a friend who got liver failure from amoxicillin-clavulanate and now she can't even drink coffee without feeling sick. It's been two years and she still cries when she sees a pharmacy. Why don't we warn people? Why is this not on every antibiotic bottle? I'm so mad. I just want everyone to know how fragile we are. Your liver doesn't text you back when it's dying.
Let us not forget the metaphysical weight of the liver as the silent sentinel of the body. To administer antibiotics without monitoring is not merely negligence-it is a metaphysical affront to the sanctity of organic equilibrium. The R-ratio, that elegant mathematical whisper of hepatic discord, reveals not just pathology, but the fragility of human hubris. We weaponize biology without reverence. And now, the body pays the price in bilirubin and bile ducts choked with silence.
Anyone else notice how no one talks about how long you're on these drugs? Like yeah amoxicillin for 5 days? Fine. But 14 days of piperacillin in the ICU? That's not treatment that's a gamble. I'm not a doctor but I've seen it. If you're on it longer than a week, get your labs done. Seriously. Just ask. Don't wait until you look like a yellow ghost.
This is one of those topics that should be taught in high school biology. We're taught how antibiotics kill bacteria, but not how they can quietly break your body from the inside. The liver is the unsung hero of your system-it filters everything, cleans the blood, makes proteins, stores energy. And we treat it like an afterthought. If you're on antibiotics longer than a week, get a baseline blood test. Check again after 7-10 days. It takes 5 minutes. It could save your life. You're not being paranoid-you're being smart. Your body deserves that much respect.
Everyone's acting like this is new news. Newsflash: this has been documented since the 80s. LiverTox has been around for decades. The real problem? People think their doctor knows this stuff. They don't. Most GPs think 'antibiotics are safe' until someone turns yellow and they scramble. And don't get me started on supplements. Milk thistle? Please. It's a placebo with a fancy label. The only thing that works? Stop the drug. Period. No magic herbs. No prayers. Just stop.